Everyone loves to chat about food. We’ll even make small talk with strangers about what we put in our mouths. Yet, we rarely discuss what happens on the other end. When we do, it’s usually in private, with doctors or close family members.
It might be taboo to talk about poo, but I’m going to break the silence, much like AJC reporter Nedra Rhone, who recently broached the topic of menopause in her Real Life column, because menopause is a fact of life.
Another fact of life: The U.S. Preventive Services Task Force recommends that people at average risk of colorectal cancer get screened starting at age 45, instead of 50, as previously advised. “It used to be just African Americans at age 45, now it’s everybody,” said Dr. Jennifer Curtis, a gastroenterologist on staff at Metro Atlanta Gastroenterology and chief of gastroenterology at Emory Saint Joseph’s Hospital.
By lowering the screening age, doctors hope to prevent and detect colorectal cancer among young people. “Younger people who tend to get colon cancer tend to get more aggressive tumors,” Curtis explained. Those with a family history of colorectal cancer should get screened beginning at age 40, or when they are 10 years younger than the age at which a family member was diagnosed with colon cancer or polyps.
Colorectal cancer is the third most common cancer in the U.S., and the second-leading cause of death among cancers. It was a shock when actor Chadwick Boseman, known for his portrayal of T’Challa in “Black Panther,” succumbed to colon cancer last year. Nearly 53,000 people in the U.S. are projected to die of colorectal cancer in 2021. Yet, it is one of the most preventable, treatable and often curable of cancers, when caught early.
“We are looking for polyps, which are growths. They are benign by nature, but can turn cancerous. We can take them out to prevent that from happening,” Curtis said. “That’s the goal of these screening tests — even if somebody is not symptomatic.”
During my annual physical, my primary care provider advised me to get screened, and referred me to Curtis. The whole affair — abstain from solid food for a day, drink awful-tasting liquid that induces diarrhea, get a scope probed up my backside — sounded like a sufferfest. But, one day of discomfort pales in comparison with alternative outcomes. My mother-in-law is a colorectal cancer survivor; besides surgery, she needed chemotherapy as part of her treatment, and has worn a colostomy bag for the past 33 years.
Here’s how my experience went:
7 days before procedure: A text alert went off on my phone: NO MORE SEEDS, NUTS, WHOLE-GRAIN BREAD OR POPCORN STARTING TODAY. I’d been instructed to avoid eating the above foods for the week leading up to the big day. None of the colonoscopy veterans I queried had been told to do that. My husband told me I should look for a new doctor. I told him he was full of it. Curtis told me that those tiny foods are harder to clear out of the GI tract, making it difficult to see when the scope goes inside. This was a team effort; I wouldn’t let the doctor down.
9 a.m., day before procedure: The Last Meal. My medical cheat sheet directed me to eat a low-fiber breakfast, suggesting low-fat yogurt with no fruit, hard-boiled or scrambled eggs, a bagel or an English muffin. I’d thought about this meal a lot, but I’d overslept and was running late for a tennis match. A dry, untoasted bagel, chased with a cup of coffee, is the worst last meal ever.
10 a.m., day before procedure: Another text alert reminder that I’d set for myself: NO MORE SOLID FOOD. Let the liquid-only marathon begin. The first two hours didn’t faze me; I was running around on the court and downing water in between.
1-6 p.m., day before procedure: Hunger games. I battled back with drinks: coffee, water, flavored seltzer, more water, more coffee, Sprite. Is white soda even soda? Jell-O was on the approved list, and there were packets in the pantry, but Jell-O reminds me of the gross stuff we did with food in the grade school cafeteria.
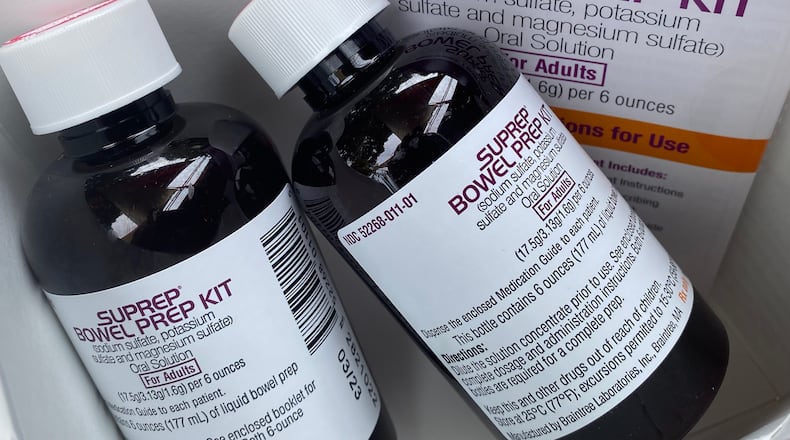
6 p.m., day before procedure: The phone pinged. Time for a first dose of Suprep! You can imagine the sticker shock when I picked up the prep kit at the pharmacy: I paid $103 to induce the runs. What a racket. I’ve done the same for my spouse and me for free, just by cooking an inedible gourd and eating one bite.
6:20-9 p.m., day before procedure: I’d scribbled a task list to keep my mind off food: Replace grip tape on tennis racket, balance checkbook, practice guitar, read. Over the course of the next few hours, I ended up doing a lot of those while indisposed. Vacuuming and laundry would wait until another day.
My husband warmed a cup of chicken broth in the microwave for me. He kindly ate his dinner in a different room. “Family members should be mindful of other family members going through these things,” Curtis had said. My husband is the best.
7:30 a.m., day of procedure: The phone pinged again: Suprep time! Did you know that the average person loses a couple of pounds when preparing for a colonoscopy?
8:30 a.m., day of procedure: Nothing to eat or drink from here on out. A colleague’s spouse happened to have the same procedure scheduled for the same day. I texted him: “Hi, colonoscopy twin. Good luck today. I can’t wait to eat something!”
“I’m fantasizing about my next meal!” he replied. Misery loves company.
10:30 a.m., day of procedure: A sign posted at the check-in desk requested that people in the waiting room kindly refrain from bringing food or drink into the area, out of respect for patients. I didn’t do myself any favors, bringing as reading material the latest edition of Gravy, the quarterly journal of food narratives published by the Southern Foodways Alliance.
Credit: Ligaya Figueras
Credit: Ligaya Figueras
11:45 a.m., day of procedure: Right before showtime, I couldn’t help but blather to my doctor about how hungry I was and describe what I planned to eat when I got home: a couple of slices of toasted Nature’s Own multi-grain bread (it’s thick, chewy and seedy), slicked with good butter and topped with a soft-boiled egg, slivers of pickled red onion, tomato slices, a sprinkle of salt and a few cracks of black pepper, and a bowl of fresh blueberries and watermelon chunks. Curtis said she’d never had a patient be so specific about their post-screening meal. The anesthesiologist shot a propofol cocktail into my veins. That shut me up right quick.
1:30 p.m., day of procedure: As I ate my best first-post-colon-cancer-screening meal ever, I looked at the images that my doctor gave me. I’ll store them with the ultrasounds from my pregnancies. Milestones, each and every one.
For more information about colorectal cancer and how to prevent it, visit gi.org. Various screening options exist. Talk to your doctor about which screening option is right for you.
Read more stories like this by liking Atlanta Restaurant Scene on Facebook, following @ATLDiningNews on Twitter and @ajcdining on Instagram.
About the Author
Keep Reading
The Latest
Featured