In what some see as a commentary on prison healthcare in Georgia, the state’s tab to settle lawsuits involving two of its former prison doctors grew in the past year to more than $3 million — and there’s a chance the figure could grow even more in 2019.
The settlements came in five lawsuits alleging negligence or deliberate indifference on the part of Dr. Yvon Nazaire and Dr. Chiquita Fye, with a sixth involving Nazaire yet to be resolved.
Although neither Nazaire nor Fye remains in their positions, critics say Georgia is still failing to live up to its legal obligation to provide adequate medical treatment for those it incarcerates.
Historically, Georgia has operated one of the most underfunded prison healthcare systems in the nation, and, even with significant increases in the last few years, it remains below the national average.
Dr. Timothy Young, the physician who has become an outspoken critic of Georgia's correctional healthcare policies since leaving his job at Augusta State Medical Prison earlier this year, said the state likely wouldn't be paying $3.1 million to settle lawsuits if it used a similar amount to hire better doctors.
“It’s just symptomatic of how disgustingly mismanaged that system really is,” he said.
Joan Heath, the director of public affairs for the Georgia Department of Corrections, did not respond to an email seeking comment on the settlements.
Inmates frequently file lawsuits about issues related to their healthcare, but they typically aren’t represented by attorneys and the cases often don’t move forward.
The issues surrounding Nazaie and Fye were different in that attorneys were willing to take them on, seeing problems that cut deeper than usual.
"I think that the care in the Georgia prison system has been shoddy for many, many years," said Lance Lourie, one of the attorneys for the family of Bonnie Rocheleau, who died from complications of pneumonia at Pulaski State Prison in 2015. "But Nazaire and (Fye) reached a whole new level."
Nazaire, who was hired even though he had been disciplined by the medical board in New York for failing to properly care for emergency room patients, was particularly “off the reservation, beyond what we normally see,” Lourie said.
Millions to settle
The state paid $2.5 million to settle three of the lawsuits by inmates or their families who alleged negligence in the care Nazaire provided for women at Pulaski State Prison, where he was the medical director for nine years until he was fired in 2015.
In July, the state agreed to pay the parents of Mollianne Fischer $1.5 million to resolve their claims that their daughter is in a vegetative state because Nazaire and others failed to recognize a series of medical issues while she was incarcerated.
The Fischer settlement — the state’s largest for a prison lawsuit in a decade — came just four months after the state agreed to pay Rocheleau’s family $925,000 to resolve their claim that Nazaire was slow to arrange hospital care for the 58-year-old inmate, who suffered from COPD and was noticeably struggling to breathe.
Nazaire is also the subject of a pending lawsuit filed by the mother of Kimery Finger, an inmate who died at 52 from complications of diabetes after leaving the prison system. The suit claims Nazaire and others are responsible for Finger's death because they failed to care for a cut that became infected and led to the amputation of her right leg.
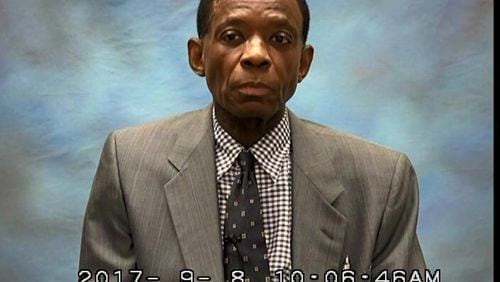
Nazaire, who now resides in New Jersey and is seeking a license to practice medicine there, was removed from his position after stories in The Atlanta Journal-Constitution in 2015 detailed how at least nine women died agonizing deaths under questionable circumstances while in his care at Pulaski State Prison and Emanuel Women’s Facility.
In the other suits, the state paid a combined $600,000 to settle claims by two men who alleged that their medical conditions were ignored by Fye, the medical director at Macon State Prison for 11 years until she resigned in 2017.
One of the lawsuits naming Fye was settled in 2017 when the state agreed to pay a diabetic inmate, Michael Tarver, $550,000 to resolve his claim that the doctor's failure to properly treat a cut on his left ankle led to the amputation of his leg.
The other was settled in February when the state paid $50,000 to William Stoner, who suffered a seizure after Fye had him placed in lockdown and abruptly cut him off from his daily dose of the anti-anxiety drug Xanax.
Fye resigned two weeks after the Tarver suit was settled but steadfastly denied doing anything improper in either case.
A daylong "site visit" at Macon State Prison by two state officials concluded that there was no evidence of inadequate care in Fye's treatment of inmates. However, it did not appear as if the officials interviewed former employees or inmates or reviewed medical records.
Lagging behind
Nazaire and Fye were among the 50 physicians employed by Georgia Correctional HealthCare, the branch of Augusta University that contracts with the Department of Corrections to provide medical services in the state’s public prisons.
The arrangement, in place since 1997, requires the Department of Corrections to pay a portion of its annual legislative appropriation — about 80 percent — to Georgia Correctional HealthCare. Georgia Correctional HealthCare, in turn, provides staffing, drugs and other medical services in the prisons.
A study by the Pew Charitable Trusts in 2017 ranked Georgia 43rd out of 49 states in annual healthcare funding per inmate. Using data from the 2015 fiscal year, the organization said Georgia spent $3,610 per inmate. Only Louisiana, Alabama, Nevada, Indiana, South Carolina and Arizona spent less, according to the study.
Since that time, records reviewed by the AJC show Georgia has upped that figure by nearly $1,000 per inmate, but the state still falls below the median of $5,720 calculated by the 2017 Pew study.
In its appropriations request for the 2020 fiscal year, the Department of Corrections has asked for an additional $20 million. However, the request is related to anticipated increases in costs for dental care and mental health services and not for the services provided by Georgia Correctional HealthCare, Heath said.
Asked why the department wasn’t seeking more funds for basic medical care, Heath responded that the department has received more than $57 million in additional funding for physical healthcare since fiscal 2017.
A dire prediction
The system is likely to come under a microscope in the coming year due to a whistleblower lawsuit Young filed in November.
Young claims officials with the Department of Corrections and Georgia Correctional HealthCare forced him out of his job because they suspected him of providing information to the AJC about the conditions at Augusta State Medical Prison, the state’s flagship prison medical facility.
He also asserts that he faced obstacles in doing his job after repeatedly raising issues of “budgetary concern,” including a lack of adequate technology and excessive delays in the approval of referrals to specialists.
In a recent interview, Young said the state struggles to hire qualified physicians because it won’t pay what the average general practitioner can earn. Georgia prison doctors make about $150,000 a year, about $40,000 less than the typical GP.
A 2014 investigation by the AJC found that one in five Georgia prison doctors were hired despite state disciplinary orders for substandard care and other transgressions.
Some prison physicians ignore serious problems or simply can’t see them, Young said. That, he said, drives up costs because those patients require more expensive treatments down the line.
“That’s just a logical line of thinking, and you see it in the real world as well,” he said. “If you’re competent on the front end, that’s how you save money.”
Young predicted more lawsuits and large settlements unless the system is overhauled.
“The system is set up to attract the dregs, and that’s what it gets,” he said.
Why it matters
The U.S. Supreme Court ruled in 1976 that prison inmates have a right to adequate healthcare. Deliberate indifference to inmates’ medical needs violates the Eight Amendment of the U.S. Constitution, which prohibits governments from imposing cruel and unusual punishment. Prison reform advocates and the Georgia Department of Corrections also have recognized that providing adequate healthcare can reduce recidivism.