Growing up, Blaze Eppinger always wondered where the medical breakthroughs for sickle cell were.
Eppinger, 33, who lives with sickle cell disease, says he has seen funding and medications surface for other conditions, which makes him and many others living with sickle cell feel like an afterthought. Estimates are that nearly 100,000 Americans, most of whom are Black, have the disease.
“As a person living with sickle cell, it always seems like we’re at the bottom of the barrel. You see other illnesses get more notoriety,” he explained. “But, not a lot of people, even in the African American community, know what sickle cell is.”
By Friday, the Food and Drug Administration will decide whether to approve a CRISPR gene-editing therapy to treat sickle cell disease. If approved, it would become the first treatment approved in the U.S. using CRISPR technology. The new treatment was approved in November by Britain’s medicines regulator.
CRISPR is an abbreviation for a family of gene sequences, and the new technology allows doctors to edit a patient’s genes to eliminate a faulty genetic code that causes sickle cell.
For Eppinger and others the news is exciting, but they wonder if the treatment will be accessible and affordable to the community suffering with the disease.
He has learned to self-manage the pain of his condition. Severe pain riddles the lives of those living with sickle cell, often leading to many emergency room or hospital visits, sometimes multiple times a year, to manage crises. Many are unable to work, exercise or do other things to lead a normal life.
With an estimated cost of about $2 million, the CRISPR treatment isn’t cheap, but is the first to offer a potential cure to those who would otherwise spend a lifetime suffering from the disease. It isn’t clear if insurance companies will cover the treatment cost.
The treatment under consideration by the Food and Drug Administration, known as “exa-cel,” uses a type of gene therapy called gene editing, which corrects a patient’s cells with genetic errors.
It requires doctors to take bone marrow and stem cells out and treat it in a laboratory setting before returning it to the patients. The procedure requires a month-long stay in the hospital, but could replace blood transfusions and other older treatment options.
Eppinger recalled the excitement he felt when he learned about a different new drug that was introduced to manage sickle cell symptoms. His excitement waned when he discovered that the treatment costs $15,000 each month.
“That’s not access to me. Just because it is available,” he said. “I don’t think availability equals access.”
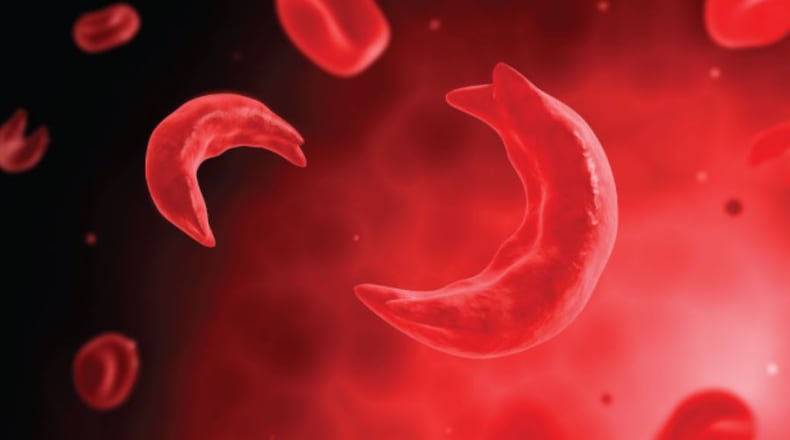
Video: Understanding Sickle cell
Sickle cell is a disease caused by one wrong amino acid in hemoglobin that causes normally round red blood cells to be shaped like a sickle, meaning they clump and clot as a result.
In addition to blood transfusions, traditional treatments for sickle cells have involved stem cell or bone marrow transplants, which carry risks and may not work. According to the American Society of Hematology, the median life expectancy for people with the disease is 42 to 47 years, compared to 76 years overall in the United States.
Tabatha McGee, executive director of the Sickle Cell Foundation of Georgia, says that the burden of sickle cell on patients has not shifted much since the founding of the organization in 1971.
“The climate [of sickle cell care], in itself, is the same by way of how the patients are treated,” she said. “However, there are many new therapies and medications that are now becoming available that can help with the day-to-day management of the sickle cell disease.”
She said many sickle cell patients are uninsured, and may be treated with suspicion when seeking pain medications during crises.
McGee estimates that it costs Georgia $16.8 billion a year to treat the nearly 14,000 people living with sickle cell in the state.
Danina Battle, manager of community health workers for the Sickle Cell Foundation of Georgia, oversees community outreach efforts to reach people living with sickle cell across Georgia. Battle says that her patients are open to any treatment that can cure them of their pain, but there are concerns around cost and safety.
“A lot of my clients will not be able to access this treatment from an affordability standpoint,” said Battle. “Yeah, it’s groundbreaking. It’s good. But, what good is it actually doing if it is not accessible to the individuals that really need it?”
Dr. Elizabeth Stenger, a pediatric hematologist and oncologist at the Aflac Cancer and Blood Disorders Center of Children’s Healthcare of Atlanta, says the health care system has been able to work through making other costly therapies affordable and accessible to patients.
“I think it’s not a matter of if, it’s just when. I know that progress has been made,” she said.
“Hopefully what work has been done for other products will make it easier for us to get these sickle cell products to a place where we’re able to offer them to patients,” Stenger said.
Keecilon Wright, 41, is a community health worker at the Sickle Cell Foundation of Georgia. Wright also lives with sickle cell. Rather than engage in drug therapies to manage her condition, she has opted for a holistic approach.
Asked by The Atlanta Journal-Constitution if she would participate in the treatment if made available, Wright said, “No, I would not.”
“I live a more holistic life and that has really helped me to minimize my hospitalizations.” She says that she has avoided hospitalization for nearly nine years through a combination of practices such as acupuncture, massage therapy, adequate sleep, mindful eating and proper stress management.
Wright said she still has questions about the new technology and its safety. “Have you had the trials to make sure that this is effective for all different types of people living with sickle cell disease and what are the consequences?”
The Atlanta Journal-Constitution and Report for America are partnering to add more journalists to cover topics important to our community. Please help us fund this important work at ajc.com/give
RESOURCES AND SUPPORT
Sickle Cell Foundation of Georgia: sicklecellga.org
Sickle Cell Reproductive Education Directive (SC RED): sicklecellred.org
About the Author
Keep Reading
The Latest
Featured