City and health officials are examining ways to bolster a safety net system that is already showing strain from Atlanta Medical Center’s impending November 1 closure.
The local government has not yet announced a plan to replace the network of care that AMC in downtown provided. Not only will the hospital close, but also many of the primary and specialty care medical offices connected to the major provider of care for Atlanta’s underserved communities.
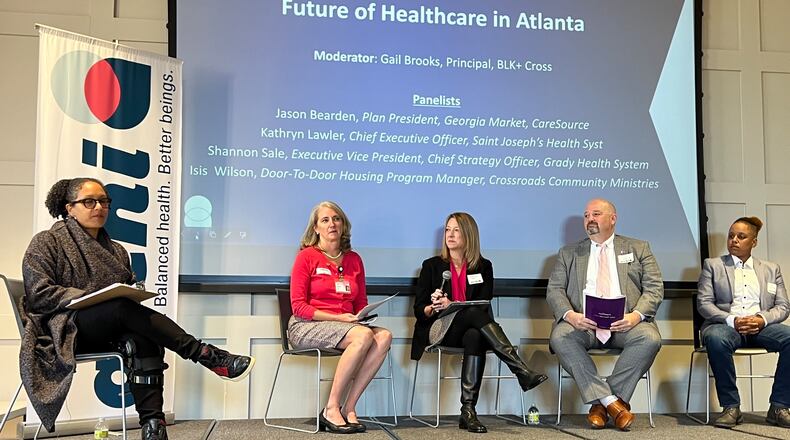
Lisa Gordon, chief operating officer for the city of Atlanta said city officials have been working with health care and community leaders in Clayton, DeKalb and Fulton counties, which will all be affected by Wellstar’s decisions to close the downtown hospital and its sister hospital, AMC South in East Point. The work was discussed at a meeting Friday morning of the Atlanta Regional Collaborative for Healthcare Improvement (ARCHI).
“It is critical that we make sure our residents, our visitors, people who love Atlanta, have access to care,” Gordon said. “Not just in existing roles, but what does the future look like?”
According to Gordon, the city of Atlanta has also turned to an outside consulting firm, Ernst & Young, to help tackle the issues that will result from the loss of medical providers.
Advocates say that Atlanta has too many resources to continue to have people struggling to be healthy. They also believe that medical providers should invest in the communities to ensure social needs are met because if a person is struggling with food, housing, employment or others needs, health care is not a top priority.
At Mercy Care, a federally qualified health center that is part of Saint Joseph’s Health System, CEO Kathryn Lawler reported a record number of walk-ins since Wellstar Health System, AMC’s owner, announced plans to close the downtown hospital. Federally qualified health centers or clinics such as Mercy Care provide care to underserved communities regardless of a person’s ability to pay.
“We need to have a conversation, right now, about what it takes to be healthy,” Lawler said. “We need to change our expectations about community health.”
Mercy Care is in the process of building affordable housing next to their clinic and headquarters. The organization hopes that their effort will set an example and help steer others to invest in changing how health care is thought of.
“If the money flows in the same direction it always has, we are going to get the same results,” Lawler said.
Emory University Hospital Midtown, Grady Memorial Hospital and Piedmont Atlanta Hospital all reported severely crowded emergency rooms on Friday afternoon, just one week after AMC’s emergency department was closed.
Credit: JOHN SPINK / AJC
Credit: JOHN SPINK / AJC
Shannon Sale, executive vice president and chief strategy officer of the Grady Health System, says that Grady’s trauma patients have increased by 20% following AMC’s emergency room closure. She believes that other patients will trickle in as time goes by.
“I think the charge is to really help systems to show up, to be there,” Sale explained. “Closing a hospital in any community is an outcome of the broader system not working.”
Others attending the meeting pointed out hospital closures are a national trend, and that this may not be the last hospital closure for the city. Leaders and advocates hope to include community members in upcoming conversations around the future of health care around metro Atlanta.
“We have a lot of work to do and it is the time to roll up our sleeves and work together,” said Gordon.
“My challenge to everyone here is to look for 21st century solutions.”
The Atlanta Journal-Constitution and Report for America are partnering to add more journalists to cover topics important to our community. Please help us fund this important work at ajc.com/give
About the Author
The Latest
Featured