Expanding Medicaid would give coverage to thousands of uninsured HIV patients in Georgia and provide millions of dollars of additional services for people infected with the virus, a recently released study says.
The expansion of Medicaid, as outlined in the Affordable Care Act, has been adopted in 38 states, but not in Georgia. Republican elected leaders who control the state government have consistently opposed the move as too costly.
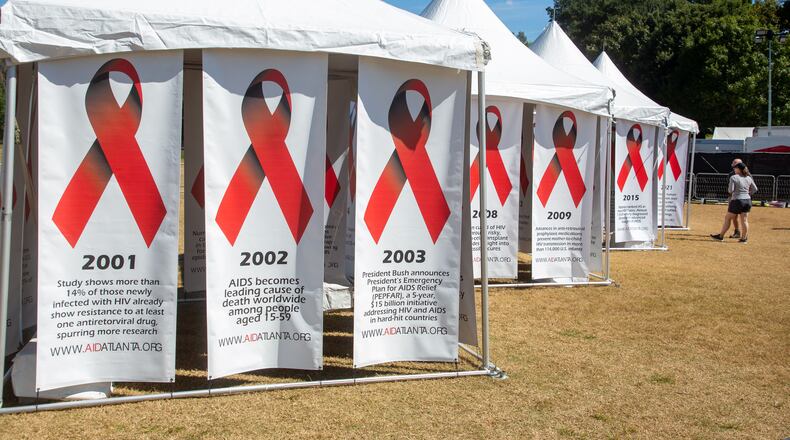
HIV, if unchecked, can lead to the disease known as AIDS, which was once almost invariably fatal. Treatment strategies now exist to block the development of the disease, allowing many infected people to live mostly normal lives.
More than 12,000 uninsured people who are currently in federal/state programs for HIV care would become eligible for Medicaid under expansion, said the study, commissioned by Georgia Equality, an advocacy group for LGBTQ individuals in the state.
That would free up $53 million in current spending to cover funding shortfalls, serve more patients and expand services, the study said.
“Looking at the result of this independent analysis proves what we have long suspected: Expanding Medicaid eligibility in Georgia to reach more people living with HIV is a cost-effective solution,” said Jeff Graham, Georgia Equality’s executive director. It would also ensure people have access to lifesaving medications now provided by the AIDS Drug Assistance Program, he added.
Such additional services, he said, “are the key to saving lives, improving health outcomes and ultimately ending the ongoing AIDS crisis.”
Gov. Brian Kemp has allocated almost $10 million in both this year’s and fiscal 2023 budget to the Drug Assistance Program, which provides medications to low-income people with HIV who have limited or no health insurance.
Georgia and the South in general are the current center of the disease in the United States.
About 2,500 were newly diagnosed with HIV in Georgia in 2019, the latest year for which figures are available. Four metro Atlanta counties rank in the top 25 areas for new diagnoses of HIV: Fulton, DeKalb, Cobb and Gwinnett.
High rates of new infections affect both rural and urban areas in the state, Dr. Kathleen Toomey, commissioner of the Georgia Department of Public Health, told state lawmakers recently.
Almost 60,000 in Georgia are currently living with the virus.
The Ryan White program, named for an Indiana teenager who died of AIDS, provides services and medical care for HIV patients who lack insurance.
The program gives grants to states, cities, counties and community-based organizations to provide care and treatment services. The goal is to improve health outcomes and reduce transmission among hard-to-reach populations.
Medicaid expansion would move most of the Georgia Ryan White patients to Medicaid, thus freeing up that funding, said the study, written by Alan Essig, former executive director of the Georgia Budget and Policy Institute.
The study also lists an alternative to standard Medicaid expansion: Developing a “waiver’' proposal for federal approval that would give Medicaid coverage to HIV patients in Georgia. That plan would also save at least $50 million and provide needed coverage for thousands, the report said.
In 2019, the CDC estimated that the average lifetime cost of someone living with HIV would be $420,285.
A spokeswoman for Kemp, Katie Byrd, said Tuesday that the Governor’s Office would need time to review the report before providing comment.
Cathalene Teahan, president of the Georgia AIDS Coalition, said extending Medicaid coverage to more people with HIV would save the state money by preventing greater medical costs down the road.
“HIV-positive individuals could obtain care and treatment, which would lead to suppressed viral loads and decreased transmission. It would give individuals an incentive to be tested.”
“Treatment is prevention,’’ she added.
Andy Miller is editor of Georgia Health News.
About the Author
The Latest
Featured