Digital health and medical technology evolved extensively during the COVID-19 pandemic, which forced health care leaders and medical professionals worldwide to find new and innovative methods to provide care, connect with patients and communicate with team members.
In addition to new technologies, the unique challenges of the pandemic paved the way for innovation and creative uses for existing technology, as clinicians scrambled to find ways to work around many new obstacles.
Which existing and emerging technologies affect nurses most? What are some of the problem-solving tools nurses continue to use during and after the pandemic?
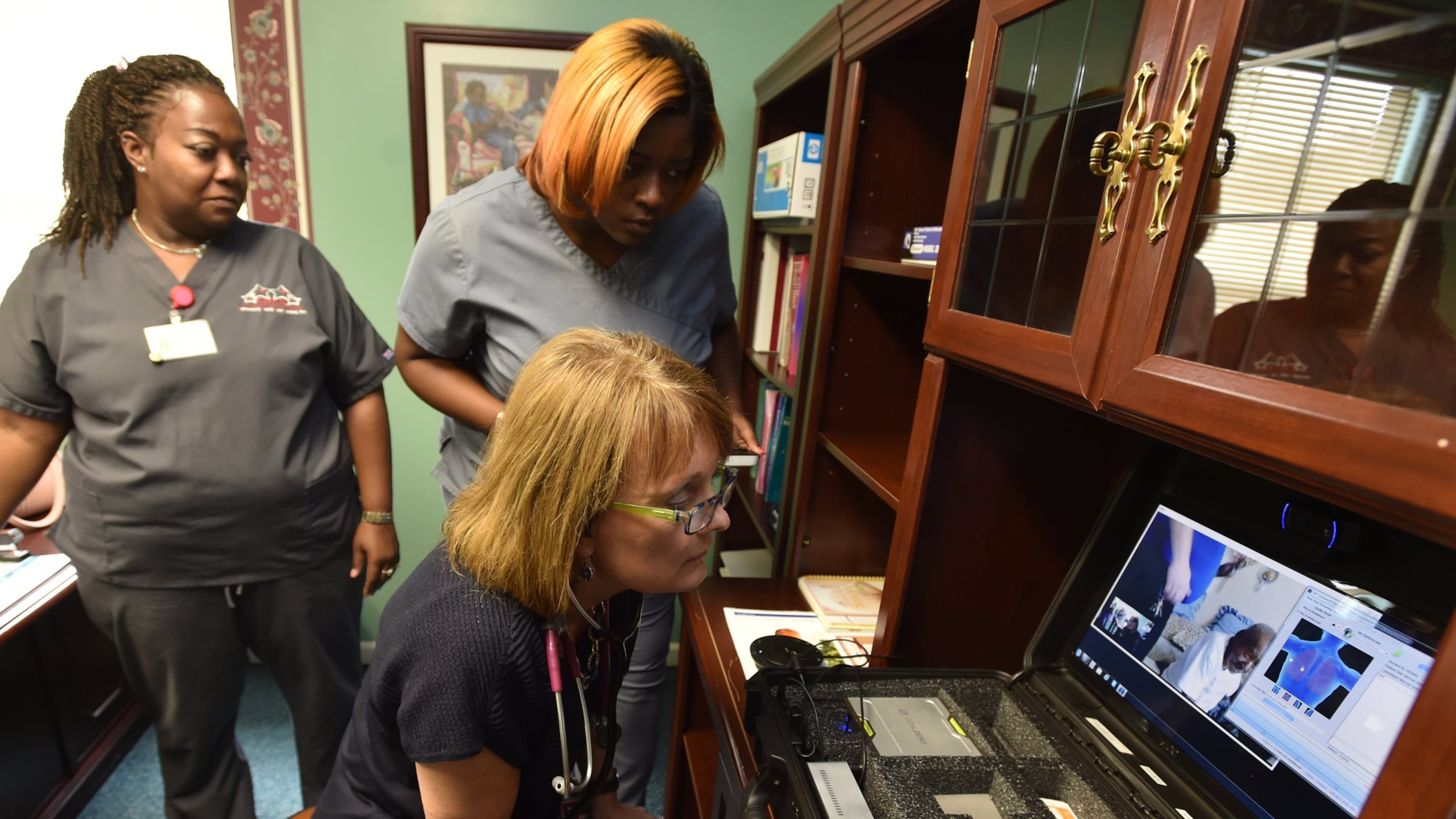
Telemedicine
Telemedicine’s popularity and use rate grew immensely during the pandemic. The CDC reports that telehealth usage reached unprecedented levels during the pandemic, citing a 154% increase in a single week of March 2020. Registered nurse Glenda Hargrove says telemedicine was a life-changer for her during the past year. “Before the pandemic, it was a luxury. Since the pandemic, it has become a necessity,” Hargrove stated.
Despite the accelerated growth of telemedicine, the future of this technology remains unclear, according to some health tech experts. While telehealth provides many conveniences, there are still some areas where improvement is needed. For example, a recent RAND Corp. study revealed the growth was disproportionately high among the most affluent metropolitan areas, while use lags in less affluent locations. Physicians and health experts insist many questions remain about the future of telemedicine post-pandemic.
Messaging, networking and teleconferencing apps
If nurses weren’t already using team messaging apps before 2020, they likely are now relying on Slack, Teams, Skype or some sort of similar app to stay connected with co-workers. Effective workplace communication during lockdowns and social distancing relied heavily on digital technology and online resources.
“We use Microsoft Teams. We have it on the computer and phones and are able to use video, share screens, have virtual patient rounds, share data in spreadsheets in ways that basic Excel does not allow,” said Regina Brigman-Lake, MSN, RN, and VP/CNO at Cancer Treatment Centers of America Atlanta. “It’s a helpful, HIPAA compliant tool for telehealth, as we use it for ICU and hospital rounds in addition to communicating between clinic teams and infusion.”
Of course, Zoom teleconferencing has enjoyed a major boom, and has even prompted new workplace lingo and etiquette. A Chicago nurse recently explained her team’s affinity for Zoom to HealthcareITNews, describing it as a lifesaver and “game-changer.” Gwendolyn Oglesby-Odom, CNO of Advocate Aurora Health, said her team uses Zoom to conduct telehealth visits through their electronic medical record software, adding that Zoom also allowed their COVID-19 patients to connect with family members remotely during lockdowns.
Virtual reality technology
Virtual reality is heavily used in gaming and occupational therapy, in addition to practical and recreational applications. The health care industry is exploring many new ways to incorporate this technology as well. With employee burnout levels reaching epic proportions across the health care workforce, VR is a valuable tool to help combat stress, anxiety and burnout among medical professionals.
Hoag Memorial Hospital Presbyterian is among the first health care facilities in the nation to deploy virtual reality therapies to support front-line workers. The launch of CenteredVR, a virtual reality-based mindfulness and stress management program developed by BehaVR, is being used as a tool to help health care workers reduce chronic stress, build resilience and enhance coping skills.
“We have seen the power of virtual reality-enabled programming to support the mental health and well-being of our patients, so it was a natural fit for us to offer a tool like CenteredVR to our nurses,” said Dr. Robert Louis, chief of neurosurgery and the Empower360 endowed chair for skull base and minimally invasive neurosurgery at Pickup Family Neurosciences Institute at Hoag. “Mindfulness practices are shown to reduce chronic stress, and CenteredVR combines those principles with the neurological and psychological power of virtual reality, offering our nurses new resources to reduce stress and improve their overall health.”
Crystal Watson, a registered nurse at Hoag, said she felt unsure about the VR technology initially. “We’ve always had other ways of dealing with stress, but none that had a visual element, so I wasn’t sure what to expect.”
Once she put on the goggles and plugged in her earphones, she said she was transported to another world, “floating high above the ocean like a bird.” As she began to use her CenteredVR regularly, her stress-induced headaches gradually began to subside, she said.
Watson was able to choose which session she wanted to experience based on the level of stress she was feeling, from on-demand options meant to target specific feelings of anxiousness, sadness or hopelessness. “I fell in love with the ‘Body Scan’ series — one minute I was on my couch stressing, the next minute I was watching a beautiful waterfall or meandering through a lush green forest,” she said.
Once she began to focus on the breathing exercises, she said the tension in her neck and shoulders began to relax. “I didn’t realize how much tension I was carrying in that part of my body until I began using the system,” she said.
While some of the nurses use the technology to decompress, Watson said she often uses it before work to prepare her for the day ahead, as it helps her to feel more in control and able to handle the stressful challenges of a 12-hour shift.
Artificial intelligence
Artificial intelligence in health care is booming, according to multiple experts and media outlets, including Business Insider, which recently reported that AI use is projected to increase by 43% from 2017 through 2023.
“AI has the ability to analyze big data sets — pulling together patient insights and leading to predictive analysis,” Business Insider reported. The report also included several ways that AI machine intelligence is performing tasks in health care that are typically associated with humans. Applications of AI in health care include determining the best treatment options for individual cancer patients based on thousands of data points, for example, as well as predicting patient outcomes via data analysis.
One additional use of AI technology is DeepScribe, a program that assists clinicians with documenting patient encounters. Co-founders Akilesh Bapu and Matthew Ko describe their product as “the first AI solution to deliver the affordability and convenience of an automated scribe with out-of-the-box accuracy comparable to human assistants.” In developing DeepScribe, creators used an approach similar to the centaur AI that recently won the American Crossword Puzzle tournament. “This approach has made DeepScribe the only AI widely accepted by medical professionals, as it can draft patient notes from natural conversation,” a company spokesperson said.
Clinicians say the DeepScribe AI program captures details they otherwise wouldn’t capture for inclusion in the transcription of the patient encounter, saving up to three hours per day normally spent on manual documentation of patient visits. “I can now knock out 48 notes in under two hours, whereas before it [would take] four or five hours,” said Nevada-based nurse practitioner Carol Cherry. “I used to spend 15 minutes per note, and DeepScribe has cut that in half.”
For more content like this, sign up for the Pulse newsletter here.