Most hospitals across Georgia fighting coronavirus have canceled tummy tucks, cataract surgeries and other truly elective procedures, but surgeons and patients face tough decisions over which surgeries can be safely delayed and which should move forward even as hospitals are in crisis mode as COVID-19 cases surge.
“Everybody agrees that trauma (surgery) doesn’t require a conversation,” said Dr. Rob Schreiner, who oversees the Wellstar Medical Group, which includes more than 1,000 medical providers working for the health system that operates 11 hospitals and hundreds of physician offices.
» COMPLETE COVERAGE: Coronavirus in Georgia
But doctors and patients will have to work through whether or not many other types of procedures will take place or be put on hold, Schreiner said.
Last week, the White House and federal health officials said all “elective, non-essential” medical and dental procedures should be delayed to help the healthcare system focus on fighting COVID-19, free up hospital beds and preserve the short supply of protective masks and gowns.
Gov. Brian Kemp said Tuesday he could eventually follow the actions some other states have taken and ban elective surgeries.
Some rural hospitals in Georgia that aren’t yet dealing with coronavirus cases continue to perform them, while many of Georgia’s largest healthcare systems announced that they were putting elective procedures off for now. But even with those announcements, there are still plenty of decisions left to make.
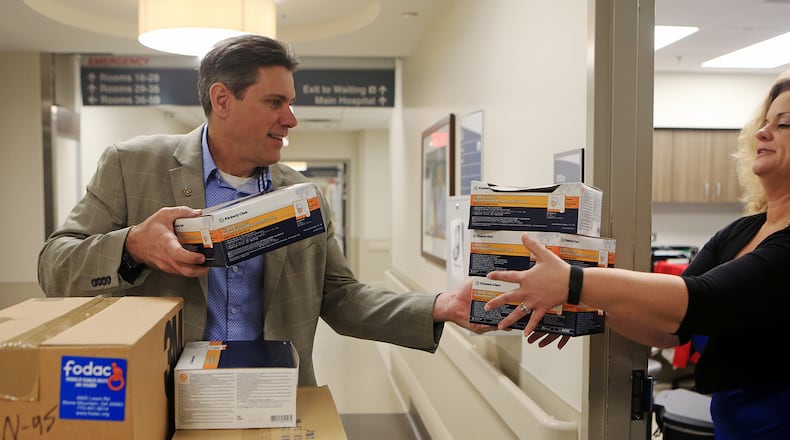
Credit: Tom Mileshko
Credit: Tom Mileshko
The federal Centers for Medicare & Medicaid Services published guidelines to help doctors and hospitals decide which procedures should move forward. That list offered examples of what should be delayed: carpal tunnel surgeries, routine colonoscopies and cataract surgeries. The guidance said surgeons and patients should consider delaying joint replacements and surgeries for low-risk cancers, while saying urgent conditions such as most cancers, traumatic injuries and urgent heart surgeries should clearly proceed.
Piedmont Healthcare said the choice is clear to proceed with cases when a patient’s life, limb or organ is threatened, and it’s clear to put on hold anything that can safely wait.
» RELATED: Clinics switch to virtual patient visits to limit coronavirus exposure
» MORE: As hospitals fight to keep up, they tell mild cases not to seek tests
But when it comes to time-sensitive healthcare issues, which fall in the middle group, Piedmont is re-evaluating each week, said spokesman John Manasso.
Healthcare systems are working through nuanced questions to determine what is actually essential and what isn’t. These are the kinds of questions, Schreiner said, that surgeons and patients are weighing: “Is it essential to the patient’s well-being? Is it essential to their chance of cure? Is it essential for their opportunity to avoid morbidity and mortality to have their operation this week versus after COVID has blown over?”
Even a diagnosis that seems the same might have a different answer for different patients. While many hernia surgeries can be delayed or avoided, pushing off some could be dangerous. That’s the case with certain breast cancer or prostate surgeries.
Credit: Christina Matacotta
Credit: Christina Matacotta
The progression of the pandemic itself may cause some of these decisions to shift. Patients will have to decide if they want to take the risk of being in the hospital where they could be exposed to the virus, even if there’s a risk associated with delaying the surgery. Plus, hospitals will have to weigh where they are with supplies, staff and beds as time goes on, and that may also play a role in which procedures go forward and which do not.
“There are all kinds of stuff in the supply chain that we have to have in order to perform a safe and effective surgery for a patient, and all of that is considered during these times,” Schreiner said.
» RELATED: Confusion, scarcity lead to haphazard testing in state's virus response
» MORE: First responders brace for strain from coronavirus
At Piedmont, the doctor and patient make an initial decision about whether to proceed with something that is time sensitive. But a small group also meets every day to review the upcoming schedule to make a final decision. “It is a rolling decision based on the available resources,” Manasso said.
Wellstar is working toward maintaining its capacity by shifting its workforce where needed, and even relying on telemedicine for patients who would normally come to the hospital or clinic for care.
There will be complexities in discussions doctors and patients will have about procedures now that weren’t a factor before the coronavirus arrived that will help determine which procedures take place, and the answers may change over time, Schreiner said.
“Do we have the supplies that we need to protect healthcare worker and patient equally? Do we have medicines that are short? Do we have surgical techs or are they home, sequestering in place?” he said, noting some issues that will have to be evaluated by every hospital. “There are these nuanced parts of the conversation in the COVID era that weren’t part of the pre-COVID era.”
About the Author
Keep Reading
The Latest
Featured