Less than two years after state officials vowed to improve conditions at Georgia’s prison hospital, the facility has been thrown into crisis again by a staffing shortage that has jeopardized the delivery of medical services for thousands of inmates.
Fueled by an exodus of dozens of experienced healthcare providers — some of whom have left due to what they describe as a toxic and retaliatory work environment — the situation at Augusta State Medical Prison has caused critical lapses in care, the state has been warned.
“I foresee significant liability risks … if there is not some sort of dramatic action taken,” the facility’s chronic care physician, Dr. Mark Taylor, wrote in a July 24 email to the risk management department at Augusta University, which provides prison medical services under a contract with the Department of Corrections.
» RELATED: Conditions make Georgia hospital breeding ground for infection
» FROM 2018: Nurses at Augusta State Medical Prison kept in the dark on asbestos
Augusta State Medical Prison was the subject of an Atlanta Journal-Constitution investigation in 2017 that exposed a myriad of unsafe and unsanitary conditions. Among other things, the AJC detailed how insects, mold and grime had made the place a breeding ground for infection and how security lapses had caused nurses to flee for their safety.
In response, state officials ordered a cleanup of the 36-year-old building, which was found to be riddled with asbestos. They also made changes in leadership, including hiring a new warden and hospital administrator.
Yet even with new management, the facility has remained in turmoil, again raising questions about the state’s stewardship of the so-called flagship of its prison healthcare system. Documents and interviews describe an environment that has driven away experienced employees on a regular basis, forcing nurses to cover shifts without doctors, physician assistants or nurse practitioners on site. Evidence suggests that when some workers have spoken out about the situation, they have faced retaliation and intimidation as a result.
Jack Evans, Augusta University’s vice president for communications and marketing, said Taylor’s concerns are under review. He said that Georgia Correctional HealthCare, the division of the university that manages prison medicine and employs medical personnel, takes all reported concerns seriously and evaluates them through proper channels.
“We have a non-retaliation policy, and employees are offered multiple methods to file reports,” Evans wrote in an email.
Regarding the staffing issues at the medical prison, he said the university has increased compensation for nurses and is actively recruiting for all open positions. Meanwhile, the university is making use of contract nursing services, he wrote.
In his email, though, Taylor painted a bleak picture. He described how the “mass departure of long-term staff” and the inability to retain newer personnel have frequently left the hospital without mid-level providers on nights and weekends.
"The administration is clueless and don't know how to treat their employees. ... I have no intention of ever stepping foot in this establishment again." —Jackie Mitchell, a nurse, in a Facebook post
In particular, he called out the current hospital administrator, Connie Melchert, and the facility’s long-time medical director, Dr. Mary Sherryl Alston, for creating a “punitive environment” that makes employees feel more like inmates “than the inmates themselves.”
“The truth is, people are willing to come here for the subpar salaries, but are turning around and leaving due to feeling disrespected, unappreciated and under constant threat of being reprimanded … for any of (an) ever growing list of possible infractions,” the doctor wrote.
When contacted by the AJC, Melchert said she couldn’t address the issues raised by Taylor without permission from the university administration. Alston didn’t respond to messages seeking comment.
Taylor sent his email just weeks after one of the facility’s more experienced nurses quit with a scathing, public Facebook post. In the July 1 post, the nurse, Jackie Mitchell, said she could no longer work at the hospital because the staffing issue had made it a “license trap.”
“The administration is clueless and don’t know how to treat their employees,” she wrote. “I have no intention of ever stepping foot in this establishment again.”
Mitchell told the AJC she was unaware of Taylor’s concerns, but she said she understands his frustration. She said her Facebook post stemmed from her own agitation over the administration’s failure to improve staffing even after she sent officials an email identifying nearly three dozen healthcare workers who had left their jobs.
“Supposedly they got rid of the asbestos and stuff like that, but the problem is (the leadership),” she said. “It’s poor leadership and poor working conditions because of the poor leadership.”
Backlash
Taylor’s email is particularly compelling because it marks the second time in two years that a physician at the facility has turned whistleblower.
Dr. Timothy Young was instrumental in exposing the filthy conditions and other issues detailed in the AJC’s articles and is now suing the university and the GDC in federal court. The doctor’s lawsuit contends that officials took retaliatory action that forced him to quit because they suspected him of leaking information to the newspaper.
» MORE: Ex-prison hospital doctor claims whistleblowing cost him his job
» FROM 2018: Settlements in prison doctor lawsuits top $3 million; could go higher
According to the lawsuit, Alston told Young after the stories appeared that his position would be “evaluated” for need, a conversation that Young interpreted to mean he was about to be fired.
Young, who headed the hospital’s outpatient clinic, was never named in the AJC’s articles but has since given the newspaper permission to identify him as a source.
Taylor declined to be interviewed for this article, but records in his university personnel file suggest that he came under unusual scrutiny after sending his email.
Three weeks after Taylor sent the email — and a week after the AJC made an open records request to obtain it — the university placed him on paid administrative leave while it investigated his reporting of an unspecified incident related to the federal Prison Rape Elimination Act. At the same time, a hospital operations analyst visited the doctor’s office to conduct an audit of his computer.
Taylor was allowed to return to work six days later but with a warning for waiting too long to report the July 31 incident and for using his office computer to watch YouTube videos and access social media, news, travel booking and entertainment websites.
The personnel records do not describe the incident in question, stating only that it dealt with the Prison Rape Elimination Act. Commonly known as PREA, the law was enacted in 2003 to set standards for the detection and prevention of prison rape.
According to a memo outlining the university’s findings and signed by Melchert, Taylor reported the incident six days after hearing about it and in fact would have done so sooner had certain officials been available. The memo also noted that the doctor had never received PREA training even though it’s required annually by the Department of Corrections.
“However, given the environment in which our patients exist, as well as Augusta University’s strong stance on a zero tolerance policy with regard to any form of harassment, it behooved you to treat the report with much more urgency than you demonstrated,” the memo states.
Wound care issues
The most serious matter detailed in Taylor’s email was wound care, a topic that has brought significant public attention to the Georgia prison system in recent years.
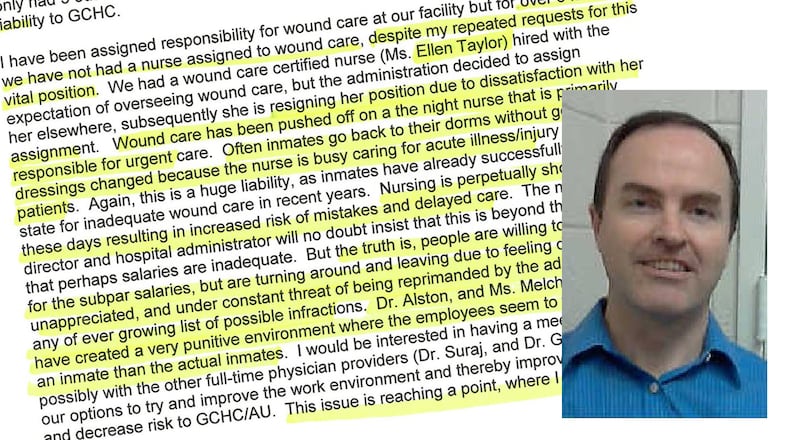
Taylor wrote that the prison hospital went six months without a nurse assigned to wound care “despite my repeated requests for this vital position” and cited the case of a nurse with wound care certification who resigned because she was never allowed to do that job.
Wound care has been “pushed off” on a night nurse primarily responsible for urgent care, forcing inmates to return to their dormitories without getting their dressings changed, the doctor wrote.
He added that failing to address the issue represents a “huge liability” and noted that some inmates have already successfully sued the state over their wound care.
The statement was an apparent reference to Michael Tarver, a diabetic inmate serving a life sentence for murder who received a $550,000 settlement in 2017 after his left leg had to be amputated above the knee after a cut became infected.
Contacted recently by the AJC, the nurse named in Taylor’s email, Ellen Taylor, said the doctor accurately described the circumstances that led to her resignation Aug. 2 after less than a year at the hospital.
The 50-year-old former Army nurse, who is no relation to the doctor, said she asked to be allowed to see wound care patients but was told by administrators that she would be more valuable teaching and working in other areas. One of those areas, she said, was mental health, for which she had no training.
“How do you say, `Set up to fail’ in two languages?” she said.
Despite the directive, Taylor said, she tried to monitor patients with serious wounds and at one point went so far as to change the orders for an inmate she saw in the emergency room. The inmate was a diabetic whose necrotic ankle wound was being treated with one wet-to-dry dressing change per day, far less than what was required, she said.
“The guy’s wound was so bad I told the (physician assistant) what to order,” she said. “The thing is, you might be a nurse, you might be a physician, but wound care is something totally different, especially diabetic wounds.”
"How do you say, 'Set up to fail' in two languages?" —Ellen Taylor, a former nurse at Augusta State Medical Prison
Taylor’s letter of resignation criticized the hospital administration for failing to follow “nursing or even GDC mandatory standards and requirements” and “blaming staff conveniently instead of taking responsibility for adverse decisions.”
“Writing in this manner does not feel right, but I have no choice,” her letter says. “The various actions are affecting the quality of patient care offered at this facility, along with smearing the (Georgia Correctional HealthCare) brand.”
`This is unsafe’
Mitchell, the nurse who posted on Facebook, said she quietly tried to alert state officials to the staffing issue almost a year before she expressed her feelings so publicly.
She provided the AJC with an email she said she sent anonymously to university and GDC officials in September 2018. The message, sent from a Gmail account set up as “fedupasmp,” identified 35 medical staff members who had left their jobs in the previous six months. In addition, it described hospital morale as “at its lowest” and noted that often there were units with only one nurse to care for more than 10 patients.
“This is unsafe and not practical even for a prison setting,” the email said. “The prison used to be a great place to work and now it’s more like a slave plantation with one master.”
Mitchell, who began working at the prison in January 2015, said her worries about staffing also led her to cut back her hours at the facility and put in more time at the Augusta VA hospital, where she also works.
Describing the night that turned out to be her last at the prison hospital, Mitchell said she found herself serving as the nursing supervisor while at the same time having to cover for an inexperienced nurse in the emergency room with no doctor or mid-level provider present.
“I had a man on the floor who had just had a seizure, somebody who was having an allergic reaction to something, people with chest pains, people coming back from the hospital — all with no provider,” she said.
She said she sent text messages to both Melchert and the director of nursing. When neither offered to send more people, she poured out her frustration on Facebook, hoping, she said, that it would bring help but realizing that it would be a major act of defiance.
“I wanted them to know that it was starting to be a danger to my license, that patients were suffering and that I had no intention of coming back because of it,” she said.
Our reporting
In a series of investigations over the past four years, The Atlanta Journal-Constitution has detailed critical problems with medical services in state prisons. The stories revealed that shoddy medical care led to deaths and injuries to inmates. At least 10 women died after their diseases went undiagnosed or they were denied adequate treatment. Another dozen inmates died of diabetic ketoacidosis after their diabetes wasn’t properly treated. The newspaper’s investigations also found that healthcare workers were put in jeopardy because of unsafe and unsanitary conditions at the state’s flagship medical prison. The coverage prompted a series of reforms. But Georgia has had to pay out millions of dollars to inmates or their families to settle lawsuits alleging that inmates were deprived of basic health care.
Keep Reading
The Latest
Featured