Is Type 2 diabetes reversible?
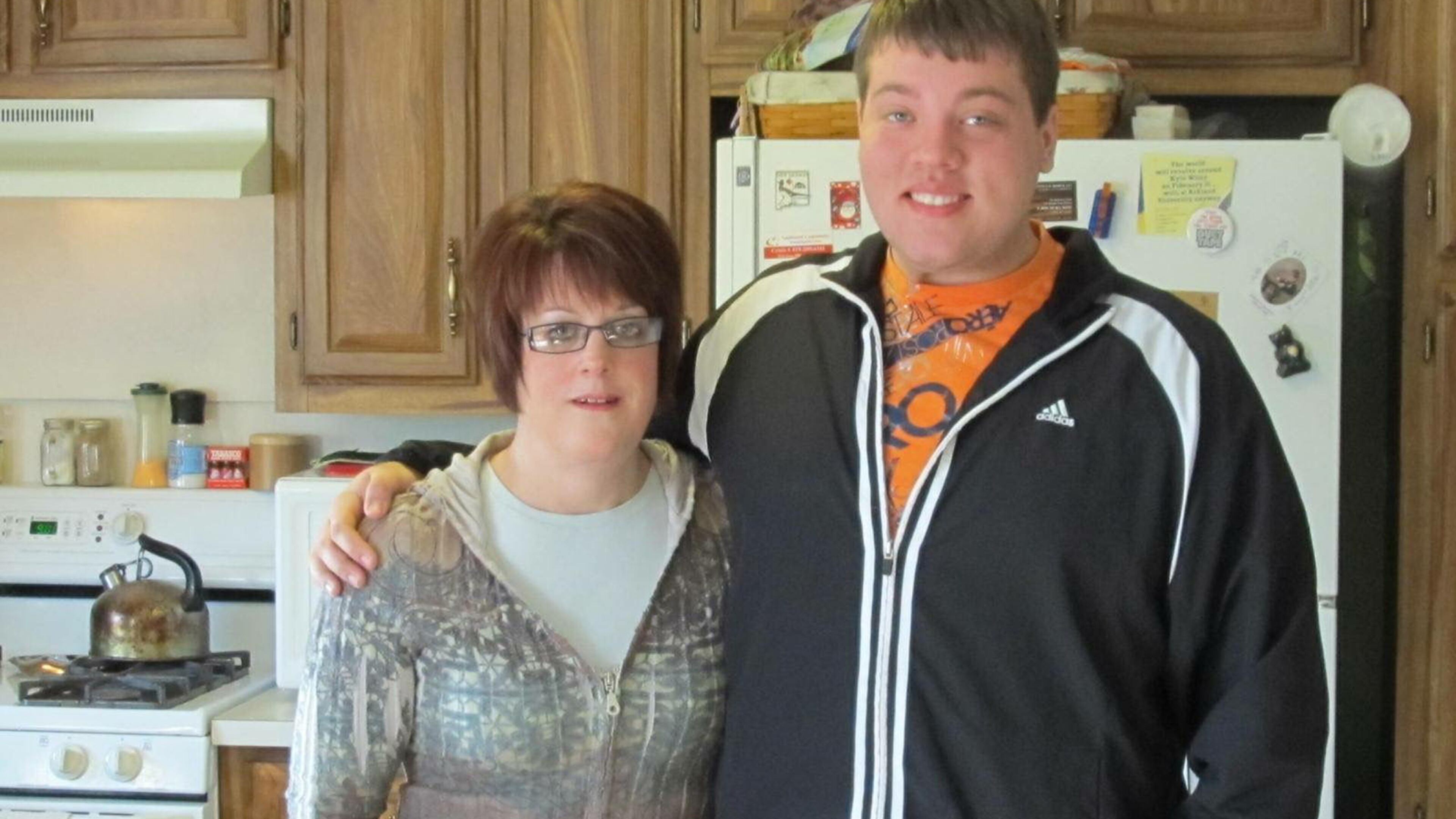
Katy Wiley began her struggle with Type 2 diabetes in 1990, when she was pregnant with her second child. The disease progressed, and at eight weeks she started insulin treatment, hoping that once her son was born, the diabetes would disappear. Instead, her condition steadily declined.
Vision problems and nerve damage, common complications of diabetes, began to appear. Her A1C blood glucose (sugar) levels were increasing, she was at least 50 pounds overweight and the medication metformin had been added to her daily therapy routine of insulin injection. That’s when she read about a Type 2 diabetes study at Cleveland Clinic that was recruiting patients to participate in one of three arms of treatments to study the effectiveness of methods to treat and possibly reverse Type 2 diabetes.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) says that Type 2 diabetes usually begins with insulin resistance or the inability of the fat, muscle and liver cells to use the insulin produced in the pancreas to carry sugar into the body’s cells to use for energy. At first, the pancreas will work harder to make extra insulin, but eventually it won’t be able to keep making enough to maintain normal blood glucose levels, and glucose will build up in the blood instead of nourishing the cells. That’s when diabetes Type 2 has developed and needs to be treated.
In the United States, according to the Centers for Disease Control, 29.1 million people — 9.3 percent of the population — have diabetes. About 95 percent of those people have Type 2 diabetes, a disease that can be prevented, reversed and maybe even cured.
“While lifestyle factors of obesity, poor diet and exercise are risk factors for Type 2 diabetes, a genetic component frequently predisposes an individual to the disease,” says Dr. Ronald Tamler, medical director of The Mount Sinai Clinical Diabetes Institute in New York.
Dr. George King, chief scientific officer at Joslin Diabetes Center in Boston says he hesitates to use the word “cure” but, with the proper diet and exercise, a person with diabetes Type 2 can go into remission for decades without treatment. King says that while we know that obesity and being overweight are major causes of the disease, only about 20 percent of people who are overweight and obese develop diabetes.
“Something is preventing the majority of overweight and obese people from developing Type 2 diabetes, and when we find out what that is, that’s when we will likely be able to find a cure,” says King.
Experts agree that the best time to reverse or prevent the onset of Type 2 diabetes is when a person is prediabetic. According to the NIDKK, a person has prediabetes when blood glucose levels are higher than normal but not high enough to be diagnosed as diabetes. A person who has prediabetes is not only at increased risk for heart disease and stroke, but for developing Type 2 diabetes within 10 years.
Dr. Brandon Colby, a prominent California physician who practices personalized age management medicine, says prediabetes can initially show no symptoms or can cause dizziness and fatigue. As a person gets closer to a Type 2 diabetes diagnosis, he says, numbness and tingling or the feeling of pins and needles in the fingers and toes may begin, a sign that the body is having trouble processing sugar.
“Physicians normally don’t pay attention to prediabetes,” says Colby, “but patients should insist they be tested for it, so that they can begin to reverse it by changing diet, increasing exercise and being warned about complications of the disease.”
The Diabetes Prevention Program (DPP), a seminal NIH research study, was a multicenter research initiative that worked with overweight participants whose blood sugar levels were higher than normal but not high enough to be diagnosed as diabetes Type 2 and who had risk factors for diabetes. Each participant tried one of three methods for preventing or delaying the onset of the disease.
The first group was a lifestyle intervention group that was trained in diet, physical activity and behavior modification to lose 7 percent of their body weight and maintain the loss. The second group took 850 milligrams of metformin, an oral diabetes medication twice a day, and the third group took a placebo pill instead of the metformin.
Dr. Aaron Cypess, clinical investigator at the NIDDK, says the study showed that weight loss and exercise for people at risk of diabetes Type 2 significantly prevents or delays the onset of disease, as does the drug metformin. A 10-year follow-up showed that prevention or delay of diabetes was most persistent in the lifestyle group.
Cypess says the study indicates that early stage Type 2 diabetes can be reversed and that early stage prevention is also effective. “When blood sugar is still close to normal, no pills are being taken and no insulin or other drugs are being used, a reversal has taken place, but the longer one has had diabetes, the less likely it is that it can be reversed,” he adds.
Dr. Philip Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute and professor of surgery at the clinic’s Lerner College of Medicine, defines remission as five years with normal blood sugar and no medication. He says the only treatment that has been able to meet the American Diabetes Association (ADA) definition of cure, published in the American Diabetes Association journal Diabetes Care, is bariatric surgery.
When Katy Wiley learned about Schauer’s pending diabetes Type 2 research trial, she took a chance that she might qualify, and she did. Once the initial testing was completed to determine her eligibility, she was randomly assigned to the gastric bypass therapy group. The other groups included one in which patients received intensive medical therapy only, including medication and counseling, and one that received sleeve gastrectomy, a different bariatric surgery procedure.
The trial, STAMPEDE (Surgical Therapy and Medications Potentially Eradicate Diabetes Efficiently), is one of the largest randomized trials with one of the longest follow-ups comparing medical therapy with bariatric surgery. It found bariatric surgery to be the most effective in reversing Type 2 diabetes.
“At the five year follow-up, a significant percentage of bariatric surgery patients had met the ADA’s definition of cure,” says Schauer.
In June, Diabetes Care devoted an entire issue to the guidelines for eligibility for the bariatric surgery. Schauer says it’s important to understand, though, that the first recommendation for Type 2 diabetes treatment is exercise and diet, followed by the addition of insulin and other drugs.
“Only after lifestyle intervention and medical therapy have been proven to be unsuccessful, is surgery recommended,” says Schauer. “And the risks of complications or death,” he adds, “are low — about as safe as the risks for procedures like gallbladder surgery and hysterectomy.”
A pioneer in the use of bariatric surgery to treat severe diabetes and not for losing weight, Wiley would not today meet the criteria for having Type 2 diabetes. In the last seven years, her blood sugar remains normal and she has taken no medication. Another 200,000 Americans are now having this surgery each year.
Schauer says that because the procedures are so successful and appear to change people’s lives, he would like to see more people qualifying and more insurance companies participating.
“I believe it will happen — more insurance companies will begin to cover the surgery, even for patients who have mild obesity like Wiley,” says Schauer. “It costs $8,000 a year to take care of someone with Type 2 diabetes and $20,000 for a one-time operation, meaning that a person who has had surgery will have successfully reduced the cost of treatment for diabetes.”
While great strides have been made in the treatment and reversal of Type 2 diabetes, more work needs to be done to prevent its onset. With better education stressing the importance of exercise, healthy eating and weight control, fewer people would need to make serious decisions about treatments for what is often a chronic, life-shortening disease.

