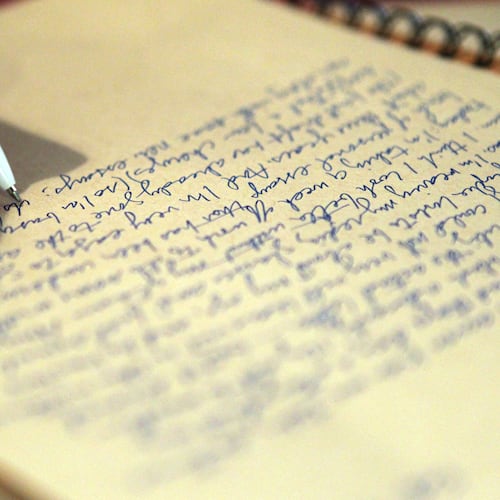
One year ago, today, I wrote the note pictured below to my husband Michael. He and I are both nurses. He works in the emergency department and I’m the outreach manager for cardiothoracic surgery.
We had just gotten through the first big COVID-19 wave and we were bracing for the next one. At the time, I had been reassigned to research and was working on two COVID clinical trials. For months, I spent most of my days in the COVID ICUs with the critical care teams caring for increasingly sicker patients. A devastating experience that I’ll carry with me for the rest of my life.
Credit: contributed
Credit: contributed
Michael and I work at different hospitals. He knows the surgeons I work with, but he doesn’t know them the way I do. They are my guys -- my surgeons. I’m so fortunate to be surrounded by such brilliance and humility and to work for such a world-renowned academic medical institution. I wrote the note because I knew that my surgeons would be my lifeboat. If through caring for the critically ill, I became critically ill, then I wanted my guys in charge of my care so Michael could be a husband and a father.
This was the reality of COVID-19 a year ago.
A year ago, I had hope that the war would come to an end and life would eventually get back to normal. I’m optimistic by nature, so I’ve tried to stay positive this entire time. Despite all the positive progress we’ve made with therapeutic drugs, diagnostic tests, hand-washing, mask-wearing, and most importantly the vaccines, we’re at the exact same spot we were a year ago, but worse.
A recent day was one of the longest days of my life. A very dear friend of mine reached out to me because her family member has been hospitalized and critically ill with COVID-19. Her family member has no medical history because he is in his 20s -- 27 years old, but did not get vaccinated. This friend of mine is pretty much family. She and her husband are nurses and introduced me to Michael. When she called, I did exactly what I would have done for my family. I reached for my lifeboat.
The doctors on my note aren’t just surgeons. They are the chief of vascular surgery, the chief of cardiothoracic surgery, the director of Emory’s Heart and Lung Transplant Center, the director of Vascular Anesthesiology and Critical Care and both of the Directors of Emory’s Aortic Center. I think it’s safe to say my lifeboat has some influential people in it. So, one by one, I called all of them. One by one they made recommendations, phone calls, etc. Eventually, one by one, they hugged me and said they were so sorry. There was nothing they could do. We have no hospital beds and we have a shortage of nurses.
It was a reality I wasn’t ready to face. This entire time, I’ve heard “no hospital beds, shortage of staff, etc.,” but I thought that didn’t apply to me or the people I care most about. I’ve been on the inside this whole time. From weekly COVID status calls with the head of the National Institutes of Health to working for one of the biggest and most advanced health systems in the world. Not to mention the “D” in my cell phone takes up 90% of my contacts because of all the doctors I know and know well enough to call personally.
But the reality is that this virus knows no status, it doesn’t care about money, age, health, career, etc. Some people say it’s just a virus, but it’s not the only problem. The biggest problem is the shortage of critical care beds, nurses and equipment.
I’m sharing this with you in the hopes that it might help shed light on our current situation.
Not light from a TV personality or a government official. Light from someone who works in a hospital and sees the real situation every day.
Let me first emphasize that I wholeheartedly believe that it is your choice what you do with your body. I always have and I have always told my patients that. It is every person’s choice to get the vaccine or not get the vaccine.
I’m urging you and pleading with you to share this information. Encourage anyone and everyone you know to get the vaccine. Vaccines are safe and effective. Encourage people to educate themselves through academic resources (Emory, Mayo Clinic, Cleveland Clinic). There are three vaccine options, and the vaccine is our last hope and only lifeline now. Almost 95% of hospital admissions are unvaccinated and nearly 100% of critical patients are unvaccinated.
A year ago, if I had needed my lifeboat, I’m confident that it would have worked. Now it’s too late, but it doesn’t have to be.
People ask me all the time, “how can I help?” Here’s how you can help. Share this with anyone. I’m more than happy to discuss vaccine options with anyone, or where they can get vaccinated.
From a nurse on the frontlines, please help us.
Missy
Credit: contributed
Credit: contributed
Missy Dinos Maton R.N., B.S.N. is outreach and referral development manager, Division of Cardiothoracic Surgery, Emory Healthcare.
About the Author
Keep Reading
The Latest
Featured