Wanda Irving and Peggy Robinson are strangers who share a tragic connection.
Both metro Atlanta women lost their daughters to pregnancy-related complications.
Irving’s daughter, Shalon, 36, died of cardiac arrest from complications related to hypertension three weeks after giving birth.
Robinson’s daughter, Regan, 29, died of cardiac arrest in 2004, an hour after delivering her first child.
Their stories underscore the racial disparity in maternal mortality. Nationally, black women are three to four times more likely to die during pregnancy and delivery, according to the Centers for Disease Control and Prevention.
U.S. Reps. Alma Adams, D-N.C., and Lauren Underwood, D-Ill., recently launched the Black Maternal Health Caucus to make black maternal health a national priority and explore policies and best practices.
While the overall danger of dying from pregnancy complications is low, between 700 and 1,200 women die as a result of a pregnancy and delivery complications each year in the United States, according to the CDC and the World Health Organization. Moreover, roughly 60,000 have life-threatening experiences, according to WHO.
Some women are at higher risk.
"The health care system has not valued black women's health overall and not valued our lives," said Angela Doyinsola Aina, co-director and a lead researcher at Black Mamas Matter Alliance, a national network of women-led, community-based organizations that provide maternal reproductive health programs and services. "They are not listening to us at all, especially when we complain about any pain or ailment that we're experiencing."
Consider tennis great Serena Williams, who delivered her daughter, Alexis Olympia, by emergency cesarean section in 2017. Williams, who is prone to blood clots, developed shortness of breath the next day and told a nurse she needed a blood thinner. Initially dismissed, Williams persisted, and doctors discovered small blood clots in her lungs, Williams said.
Income and education level don’t seem to matter, advocates say.
“You can have a Ph.D., but when you come into a clinic or hospital, they automatically start stereotyping,” said Aina. “There’s more to the story than black women entering into pregnancy are not their healthiest selves. It’s the systematic racism in the health care system.”
‘Big Hole in My Heart’
Shalon Irving was a superachiever.
She earned a dual doctorate in sociology and gerontology by 25. She held degrees from Hampton, Purdue and Johns Hopkins universities.
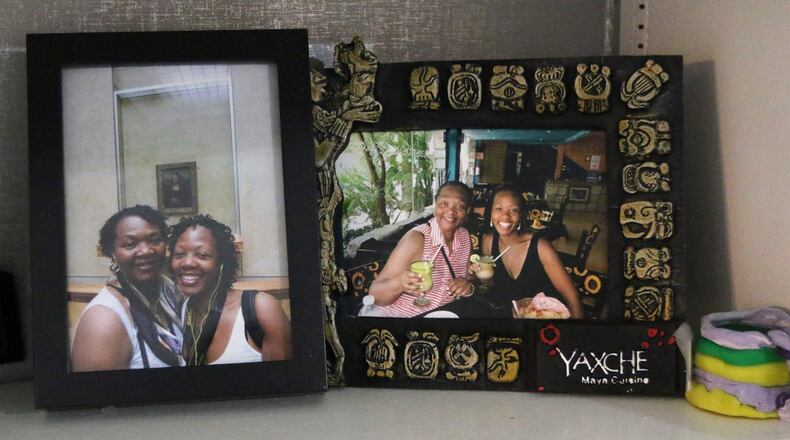
The Sandy Springs condo where her mother and daughter, Soleil, 2, now live is filled with photos of a smiling Shalon with her mother on vacation. On one shelf is a U.S. flag, folded neatly in a display case.
“Things came easy for her, but she had the kind of intelligence and brilliance that she didn’t flaunt,” said Wanda Irving. “She was warm and kind. She was my best friend.”
Her daughter, a lieutenant commander in the U.S. Public Health Service Commissioned Corps and a CDC epidemiologist, was in good health. She exercised and watched what she ate. She had a history of hypertension and a blood clotting disorder, but she’d gotten them under control and had not been on medication for several years.
Her pregnancy and the delivery by C-section on Jan. 3, 2017, went as planned.
But within a week she started feeling poorly.
She made several doctor’s visits over the next few weeks for pain and swelling at the incision site and for hypertension, according to a medical negligence lawsuit filed in May 2018 that’s set to go to trial next year in DeKalb County state court that names one of the physicians who treated her and the Emory Clinic.
A spokeswoman for Emory University, which owns Emory Clinic, said it does not comment on pending litigation.
She complained of exhaustion, abdominal pain, headaches, and an inability to urinate, her mother said. Her blood pressure rose.
On the night of Jan. 24, Shalon Irving was talking with her mother. Midway through a sentence, Shalon started making a garbled sound. Her eyes rolled back in her head, her arm rose, and she collapsed.
She was rushed to the hospital but never regained consciousness. Two days later she was declared brain dead.
At 65, Wanda Irving thought she would spend her days as a doting grandmother, taking her granddaughter to the park or the beach.
Instead, she is raising Soleil.
“I couldn’t wait to watch the two of them grow together,” said Irving, her voice quivering and tears streaming down her face. “This has left such a big hole in my heart.”
‘Everybody Is Not the Same’
Peggy Robinson shares the same grief. Her daughter, Regan, died in 2004 within an hour after giving birth.
Today, Robinson’s granddaughter, Devyn, is an outgoing 15-year-old.
“It’s been a roller coaster, but it’s also been amazing,” said Robinson, who retired from the U.S. Postal Service and is raising Devyn in Atlanta.
Devyn’s aunt, Mia, said they are waiting for the day when she asks about her mother’s absence.
That day, though, may not come for a while.
“This is her normal,” said Mia Robinson, who is helping to raise Devyn. “She has never known her.”
Regan worked as a postal clerk in Marietta when she found out she was pregnant. An avid traveler and dancer, she was thrilled about becoming a mom.
But by her third trimester, it was obvious something was wrong.
Her complexion darkened and her feet were so swollen that, at times, Regan wore slippers to work.
She was due to deliver in March. But during a routine doctor’s visit in February, her blood pressure was so high that she was sent directly to the hospital.
She was diagnosed with pre-eclampsia, a condition that can affect pregnant women and includes high blood pressure and increased protein in the urine.
Peggy Robinson said her daughter was overweight but never had blood pressure problems.
Shortly after delivery, Regan started having a seizure. Within a few minutes she went into cardiac arrest and died.
“I think when young women go to the doctor’s office, they treat everybody the same, but everybody is not the same,” said Peggy Robinson. “The doctors should have seen the signs because of her blood pressure. It had to be off the chart to admit her to the hospital.”
‘Black Women Are Not Believed’
One of the most high-profile black maternal mortality cases involves Kira Johnson, the daughter-in-law of Judge Glenda Hatchett.
On April 12, 2016, Johnson, 39, arrived at Cedars-Sinai Medical Center in Los Angeles to deliver her and her husband’s second child by scheduled C-section.
After the birth, Charles Johnson IV noticed blood in his wife’s catheter.
RELATED: Judge Glenda Hatchett and son fight for lives of new mothers
About 10 hours after delivery, her condition deteriorated and she was taken to surgery, according to a lawsuit in the case.
Her heart stopped almost immediately, but doctors were still working on Kira.
She never left the hospital.
An autopsy determined Kira Johnson died of “hemorrhagic shock due to acute hemoperitoneum,” which the lawsuit said doctors failed to properly diagnose and treat.
"We are really seeing people wake up," said Charles Johnson, who lives in metro Atlanta and is raising the couple's two sons.
He has formed a nonprofit, 4Kira4Moms, which addresses maternal mortality and wellness. "They understand that this is an issue and support is growing exponentially. This is something that can no longer be ignored."
Sequoia Ayala, director of policy and advocacy for Atlanta-based SisterLove, agreed, citing the need for better training for medical staff, support for midwifery and community-based programs, and an expansion of Medicaid.
“Part of the conversation is that black women are not believed and not given the same level of care. In the case of Kira Johnson, she had insurance, the ability to choose her own providers, and access to what should have been the best care in the world. Still, her concerns were overlooked. Why?” Ayala asked.
“All people deserve access to culturally competent, patient-centered care. Black women, irrespective of their income level, are not getting that,” she said.
About the Author
Keep Reading
The Latest
Featured