For more than a decade as an Emergency Medical Technician, James Dow, of Roswell, never had trouble finding a job. Then, the inexplicable happened: The pandemic hit, and he was out of work.
“Something’s not right here,” the 33-year-old said. “All these cases and all these people sick and dying, you would think EMS would be busy, but it’s the complete opposite.”
In the early months of the pandemic, Georgia was scrambling to find enough paramedics and EMTs to ride in the backs of ambulances. Even thousands of retired medics were asked to return to work to help address the surge of coronavirus patients. Now, months later, with people avoiding hospitals and call volumes down as much 30 percent drop, ambulance companies have lost significant revenue and are having to lay off medics like Dow or reduce their work hours.
That comes with a heavy price for Georgians, too. The cutbacks are impacting the ambulance services’ ability to be ready to deliver emergency medical transport services, particularly with coronavirus cases again climbing.
“We are gravely concerned that various factors related to this pandemic are pushing ambulance services to the breaking point,‘' Georgia ambulance executive Pete Quinones wrote to a top official at the Georgia Department of Community Health.
Every ambulance provider in Georgia is suffering the impact of the financial crisis, wrote Quinones, who is chief executive officer of the Marietta-based Metro Atlanta Ambulance Service, which serves Cobb County. “Whether your community contracts with an ambulance company, has a city or county-run service, depends on a hospital to provide ambulances or has a department ambulance program, they are facing a dramatic situation where revenues and funding are disappearing.”
While the federal government doled out more than $3 billion in relief money to health care providers, including hospitals, physician’s offices and healthcare clinics, significantly less support went to ambulance providers, including fire and EMS departments, to address COVID-19 related shortfalls. About 100 Georgia ambulance providers turned to the federal Paycheck Protection Program for loans, but many say that is only a temporary fix that will allow them to meet payroll over a few more months.
At one point, in a move to help ambulance services, the federal government issued a waiver that allowed them to be reimbursed for transports to facilities other than hospitals, such as doctor offices or clinics. But that hasn’t brought in a significant amount of new revenue as many health care providers closed to the public for weeks.
Now, the situation has become so dire, EMS leaders told The Atlanta Journal-Constitution, that they have turned to the state for assistance. In late April they made a formal request to DCH for additional reimbursements to address the disruption in their operations. The requests include additional reimbursements for ground ambulance providers that assess patients at their homes, a key point of contention in an industry that is only paid when it transports a patient to a hospital.
Leaders also want the Department of Public Health to partner with ambulance services to provide COVID-19 tests and register results.
A spokesman at DCH referred questions to DPH. Nancy Nydam, spokeswoman for DPH, did not respond to requests for comment by deadline.
Dow, who is an EMT-intermediate, said he has been looking for work for weeks. But many start-up providers have gone belly up, he said, and others aren’t hiring.
“It’s like you’re competing for a spot at Harvard,” he said. “I don’t know what’s going on. I feel like I’m in the Twilight Zone or some strange alternative universe.”
‘You could shoot a cannonball through them’
A complex chain of financial pressures affected state ambulance providers during the COVID-19 public health crisis.
In mid-March, Georgia braced for a surge in COVID-19 patients. To make room for them and free up resources, including access to ventilators and personal protective gear to treat the sick, hospitals stopped elective procedures, including surgeries, examinations and testing.
Patients also vanished from doctor’s offices and medical facilities, as many closed their doors.
“Everything was empty,‘' said Larry Richardson, executive vice president of AmeriPro EMS, a Stockbridge-based private ambulance provider that serves Georgia and Florida. “When I say empty, I mean you could shoot a cannonball through them.‘'
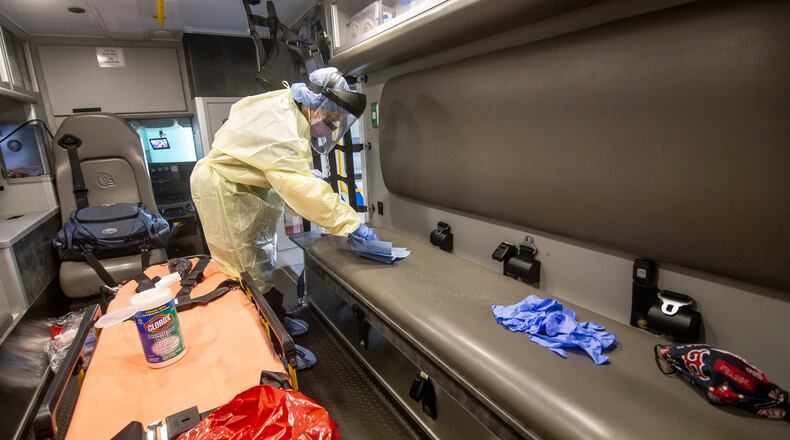
Meanwhile, as Richardson and others watched their peers in New York City ordered into isolation after exposure to the virus, they began stockpiling masks and gloves. They spent more money to purchase decontaminants and to equip their advanced life support vehicles with additional ventilators, heart monitors and gear to treat the most critically ill. Cost soared, especially, for the N-95 masks that protected medics from exposure to the virus.
“We knew we were going to be better safe than sorry,” said Chad Black, chairman of the Georgia Emergency Medical Services Association and is also the EMS director in Habersham County.
Then, an eerie silence took over the streets.
By April, shelter-in-place restrictions kept the public at home. Restaurants and bars closed. Seniors and those with compromised immune systems were urged to stay isolated. Hospitals also asked the public to avoid the emergency room to avoid the spread of the disease.
Hospital bays, where ambulances parked to deliver and pick up patients, were deserted. Emergency 911 centers received far fewer calls.
“People were nervous to go to the hospital and people were delaying care,‘' said Steve Vincent, chief operating officer for Gold Cross EMS in Augusta. “They were just not calling.”
Diving into reserves
Over the next several months, many patients who called for help refused to be transported to the hospital after receiving assessment and treatment at home, said Robby Atkins, regional president of Priority EMS. In May, his costs to deliver service to those “no-haul” patients shot up by 40 percent compared to a year ago, he said.
Also, by May, counties that fund ambulance services were digging into their reserves to find enough money to pay overtime to paramedics to replace those who had been sidelined by the virus.
“Something's not right here. All these cases and all these people sick and dying, you would think EMS would be busy, but it's the complete opposite."
In early May, Maureen Orr, EMS director in Brantley County, lost two paramedics and an EMT. Then she, herself, got sick with COVID-19. Two of the medics were hospitalized, and she had to stay in bed for two weeks. She remained calm during the ordeal, she said. She didn’t want to create a panic in a community where her paramedics provided the only medical care in 35 miles. Brantley has no hospital.
“It was already bad enough and we didn’t want to be discouraging people who had it or were sick from going to the ER,‘' Orr said.
At private ambulance companies, along with cutbacks in work schedules, administrators have taken pay cuts.
Administrative staff and management at Priority EMS, which operates Central, Puckett and National EMS, accepted a reduced salary for several months. Quinones said he took a pay cut of up to 25 percent.
Block grants sought
The goal is now to trigger more dollars from the state and federal governments under CARES to avoid more draconian measures, such as more pay cuts, furloughs, and layoffs.
One request by the Georgia Ambulance Providers Association has been to urge the Georgia Trauma Commission to release up to $29 million in block grants to support EMS staffing over the next six months.
“Without that, we don’t have the financial ability to keep a state of readiness,‘' said Terence Ramotar, director of government affairs for the southeast region for American Medical Response, the exclusive 911 ambulance provider for DeKalb County.
Black, the EMS association chairman, says the situation is untenable for an industry already in crisis.
Georgia already can’t hire and retain medics to cover demands. A key reason is that Georgia paramedics are among the lowest paid in the nation, and many exit the profession for higher-paying jobs, such as nursing.
“We throw these medics in the frontline dealing with COVID patients, day in and day out,” Black said, “then, when the big rush is over, we say we don’t need you anymore. We can’t afford to keep you. That’s unfair.”
About the Author
Keep Reading
The Latest
Featured