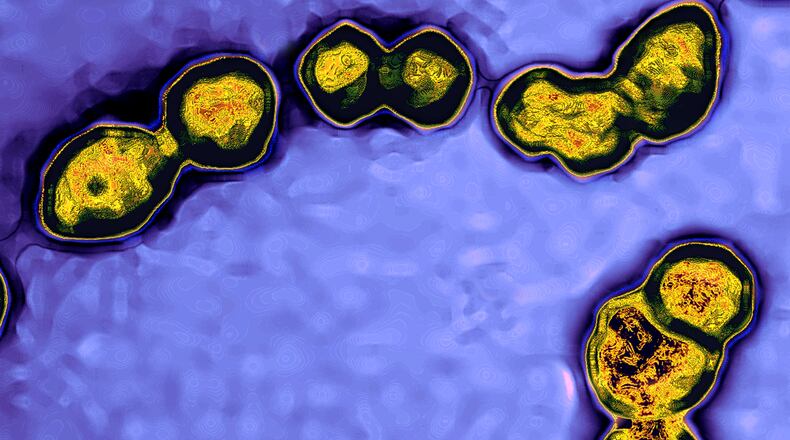
Doctors should be on the lookout for a particular kind of invasive strep infection in children that can result in so-called “flesh-eating” disease and organ failure, according to health officials.
Shortly before Christmas, the U.S. Centers for Disease Control and Prevention issued an advisory on the recent increase in pediatric invasive Group A streptococcal infections, otherwise known as iGAS.
These bacterial infections can cause potentially deadly illness such as necrotizing fasciitis — sometimes referred to as “flesh-eating bacteria” — as well as toxic shock syndrome that can cause organ failure and sepsis, an extreme and sometimes deadly bodily response to an infection. Another complication can be cellulitis, a bacterial skin infection that can lead to painful swelling.
It’s too early to know for certain whether the increase in such infections is what would be typical prior to the pandemic. But iGAS cases in children this season are above similar periods seen in the first two years of the COVID-19 pandemic. In any case, the number of iGAS infections nationally has been relatively low.
However, federal officials have been investigating a possible rise in iGAS infections in children at a Colorado hospital, and potential increases have been subsequently reported elsewhere.
In Georgia, the state Department of Public Health tracks iGAS infections and on Friday a spokesperson said the agency is seeing an uptick in cases. However, DPH was unable to release the number of cases seen recently. According to DPH guidelines, all Georgia physicians, laboratories, and other health care providers are required by law to report patients with iGAS within seven days.
The spokesperson said additional testing was being conducted on samples sent to CDC.
Meanwhile, a Children’s Healthcare of Atlanta spokesperson said they are not seeing an increase in patients with Group A strep infections, but they remain vigilant.
“Children’s recommends all children and adults get their flu and chickenpox vaccination as Group A strep can appear as a secondary infection,” the hospital system said in a statement. “Parents should consult their child’s pediatrician with concerns about prolonged or delayed onset of fever during a respiratory illness.”
Group A Streptococcus bacteria can cause more mild but still painful illness — such as streptococcal pharyngitis, commonly referred to as strep throat. Symptoms can include sore throat, pain when swallowing, fever, red and swollen tonsils, and swollen lymph nodes. Children can have symptoms that also include headache, stomach pain, nausea and vomiting. People with strep throat can also have a rash, which is known as scarlet fever.
By contrast, more dangerous iGAS infections “are associated with high mortality rates and require immediate treatment, including appropriate antibiotic therapy,” the CDC said.
Health authorities in Britain have been tracking cases of iGAS, which remain rare there. Authorities in early December reported five recorded deaths within a week of an iGAS diagnosis in children younger than 10 in England. During the last season where Group A streptococcal infections were particularly high, there were four deaths in the same age group over the same time period.
Exposure to someone with strep throat puts them at greater risk for an iGAS infection, the CDC said. Strep throat is common among school-aged children age 5 to 15, and typically peaks in the U.S. from December through April. Cases of iGAS are particularly high when flu levels are high, and this flu season is shaping up to be the worst in at least a decade.
People who are already sick with, or recently had, a viral infection such as flu or chickenpox are at higher risk for iGAS, according to the CDC. Seniors, nursing home residents, people with chronic medical conditions, those with wounds or skin disease, intravenous drug users, homeless people and Native American populations are all also considered to be at higher risk for iGAS.
The CDC is urging parents to familiarize themselves with symptoms of iGAS and seek prompt medical attention. Here’s a rundown of symptoms of the most dangerous complications:
— Necrotizing fasciitis: Early symptoms include a red, warm or swollen area of skin that spreads quickly, severe pain and fever. Later symptoms can include ulcers, blisters or black spots on the skin, change in color to the skin, pus or oozing from the infected area, dizziness, fatigue, nausea or diarrhea.
— Streptococcal toxic shock syndrome: Illness begins with fever and chills, aches, nausea and vomiting. But within 24 to 48 hours more serious symptoms develop, such as low blood pressure, a faster-than-normal heart rate, rapid breathing and organ failure. Failure of the kidneys, for example, can be detected if a person stops making urine. Liver failure can be detected if they’re bleeding or bruising a lot, and their eyes might turn yellow.
— Cellulitis: Symptoms appear as a red, swollen and painful area of the skin — commonly on the feet and legs — that’s warm and tender to the touch. “The skin may look pitted, like the peel of an orange, or blisters may appear on the affected skin. Some people may also develop fever and chills,” the CDC said.
An iGAS bacterial infection in someone who already has a viral infection of another disease may appear in a patient as ongoing or worsening symptoms after an initial improvement in sickness.
Staff writer Helena Oliviero and The Associated Press compiled this report
About the Author
Keep Reading
The Latest
Featured