Didn’t see that coming: Surprise medical bills draw scrutiny

It’s called “balance billing,” but what it does is knock consumers off their feet.
Here’s what happens:
A patient scheduled for surgery makes sure the hospital and the surgeon are in the patient’s health plan network. But after the surgery, a surprise bill arrives for hundreds of dollars.
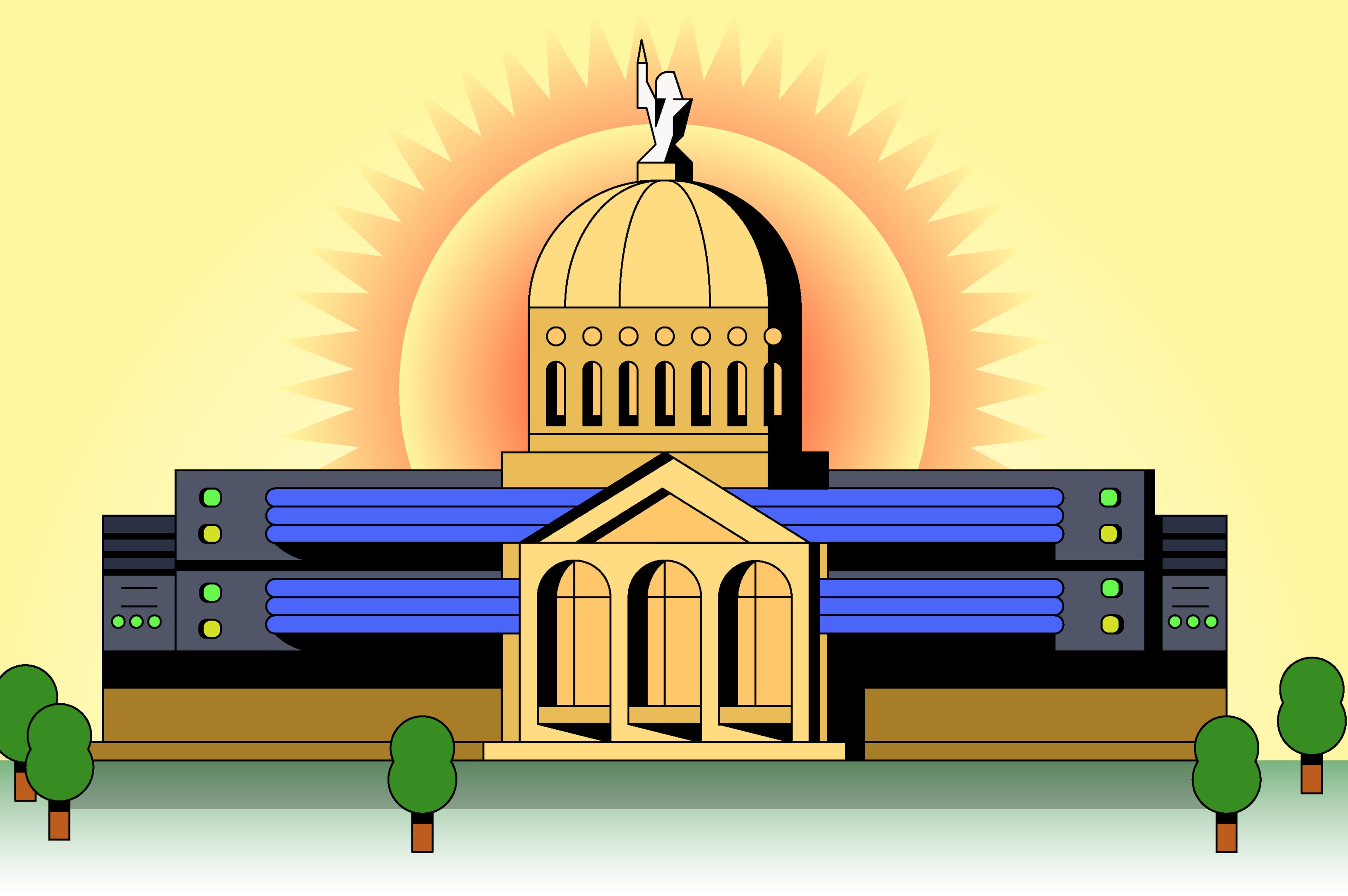
Faced with constituents complaining of medical debt, medical-bill-related bankruptcies and credit rating downgrades, a state legislative panel held a hearing recently about surprise billing for medical care.
Physicians and members of the hospital and insurance industries testified and pointed fingers of blame.
“Without protections, consumers are left holding the bag,’’ said Beth Stephens of Georgia Watch, a consumer advocacy group.
But are protections even possible? Find out the root causes of the problem and the outlook for potential solutions on MyAJC.com.