Georgia hits insurance companies with $25 million in fines
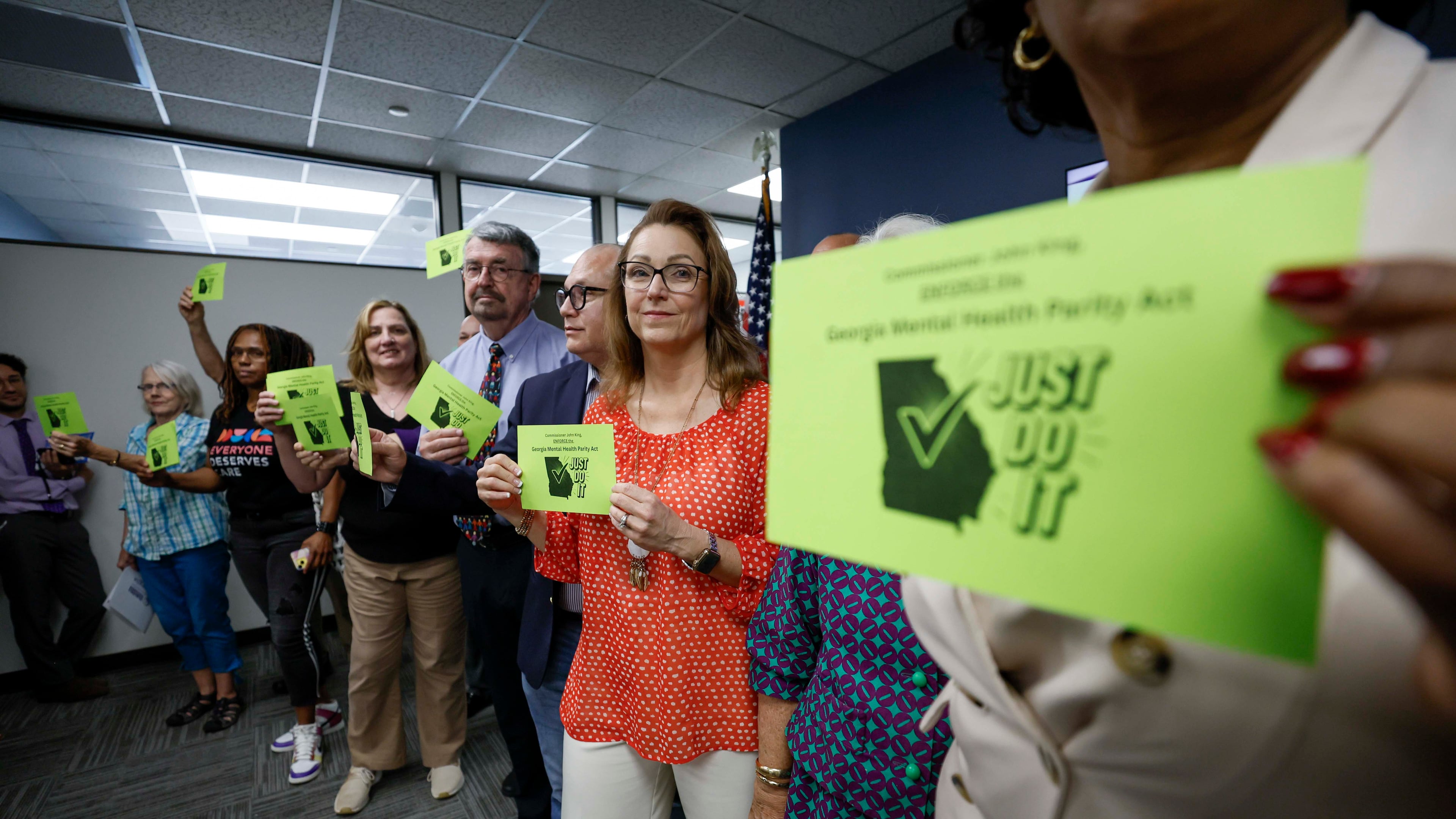
The Georgia Department of Insurance is ordering nearly two dozen health insurance companies to pay fines totaling $25 million for breaking state laws requiring them to cover mental health claims the same way they cover physical health.
Since August, when the violations were initially announced, investigators assessed $5 million more for offenses, and additional fines were levied for not responding to inquiries in a timely manner.
The 22 insurance companies fined have 60 days to request a hearing with the state agency or appeal the fines to the Fulton County Superior Court. The list of companies includes Aetna, Humana and CareSource, along with other national insurers and many smaller companies.
“These companies are not above the law, and I am taking definitive action to hold them accountable for denying Georgians the care they need,” Insurance Commissioner John King said in a statement.
King’s office discovered more than 6,000 violations of a 2022 law requiring insurers to have the same copays, deductibles and number of sessions for anxiety, depression or addiction as for illnesses of the rest of the body. The investigation found some companies were inconsistently applying benefits and requiring patients to get approval before care even when it wasn’t necessary.
“Georgians will see affirmative action to ensure the law is upheld, and we will continue to work with the community to make sure mental health is equal to physical health,” said state Rep. Todd Jones, R-Cumming, who co-sponsored the 2022 law.
The fines do not include restitution, meaning patients who were forced to pay for services and treatment that should have been covered will not get their money back. Instead, the money will be sent to the state treasury.
“OCI’s actions are a good beginning but do not yet address individuals who have been illegally denied access to medically necessary mental health care,” said Roland Behm, a mental health advocate who assisted legislators in drafting the law.
State Sen. Nabilah Parkes, D-Duluth, who is running against King for insurance commissioner, took partial credit for the fines, even though the initial investigation was started months before her campaign announcement.
“If you had told me that all I had to do was run for Insurance Commissioner for John King to do his job, I would have done it sooner,” Parkes posted on X after the fines were announced.
King has faced criticism for failing to enforce the law or create awareness of it. A 2024 report found only 13 unique complaints were reported to the state about mental health violations.
King’s office has said enforcement takes time.
“These fines were first announced last August,” King’s campaign wrote in a reply to Parkes. “Facts matter, but nice try.”
The violations occurred in 2022.
Investigators will begin examining whether any violations occurred in 2023, 2024 or 2025 and could issue more fines for those years.
“It’s not going to be another three years,” said Bryce Rawson, a spokesman for the insurance commissioner. “If we find companies violate the law again, we will hold them accountable.”



