Insurance commissioner urged to enforce mental health laws
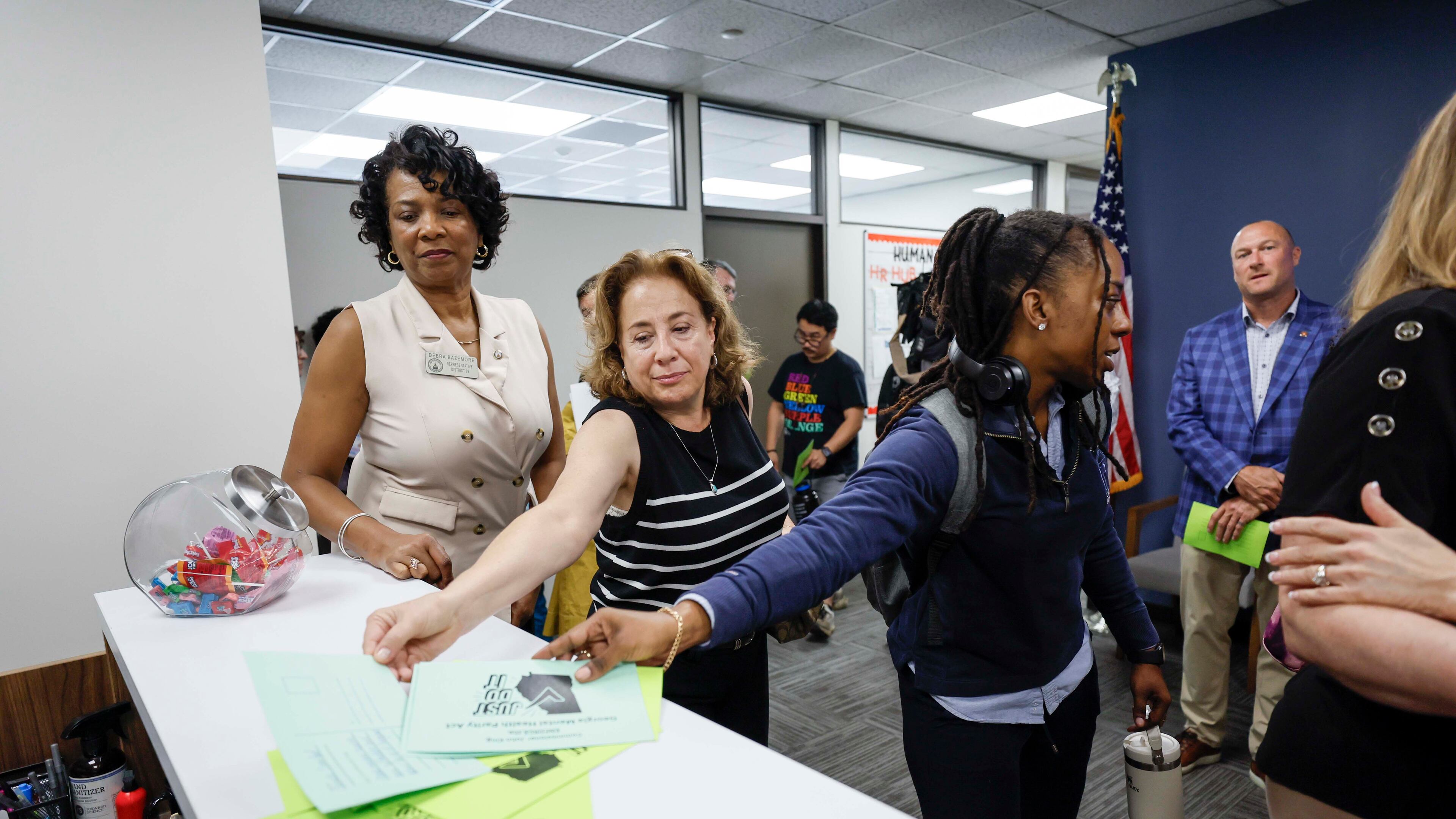
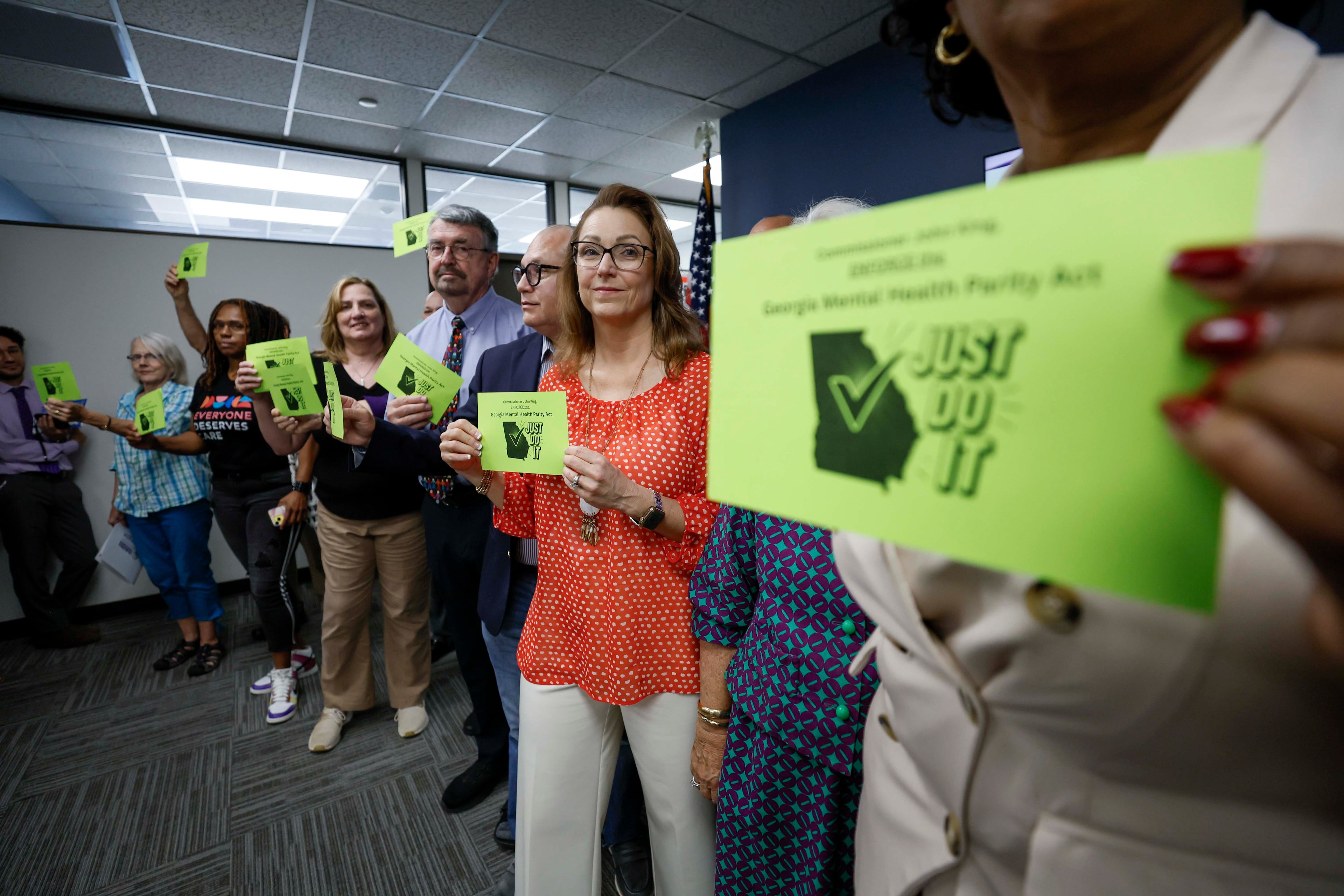
About 50 mental health advocates and state lawmakers delivered hundreds of handwritten letters to Georgia Insurance Commissioner John King’s office Monday morning, urging King to force health insurance companies to cover mental health at the same level as physical health.
The letters, plus an online petition, build on criticism that King was not adequately pushing insurers to comply with a 2022 law requiring comparable coverage or boosting awareness that the law existed. On Friday, King’s office announced 22 health insurance companies had violated the law and will pay the state a total of $20 million.
“It’s a great step forward. We definitely think there is more to be done,” said Kim Jones, the executive director of the Georgia chapter of the National Alliance on Mental Illness.

The advocates said they want assurance for health care providers who bring complaints about insurance companies that they would have legal protection if they faced retaliation from insurers.
And they want to ensure the fines imposed on insurance companies will make an impact.
Jeff Breedlove, a lobbyist for the Georgia Council for Recovery, said he’s worried that insurance companies will get into the habit of paying a fine each year instead of obeying the law.
“A million dollars, in my opinion, to a big insurance company … is nothing, but it’s everything to a working family of Georgia,” he said.
State Rep. Mary Margaret Oliver, a Democrat from Decatur who cosponsored the 2022 bill, said she will reexamine the fines insurers pay for violations, which range from $2,000 to $5,000 per violation. A bill that would have reinforced the mental health law by establishing a panel to analyze reports from insurance companies passed the state House by a wide margin but stalled in the Senate.
“As I go back to the 2026 session, that’s going to be one of my focuses,” she said.
King’s office identified 6,000 violations from the 22 insurers, including some that inconsistently applied benefits and required approval from the insurer prior to care even when that approval was not necessary.
Bryce Rawson, a spokesperson for King, said his office could not share the names of the 22 companies until documents had been finalized and approved by the department’s legal team. He also did not provide an estimated timeline for when the process would be completed.
The mental health advocates also requested a meeting with King to discuss working together to implement the 2022 law that required this coverage. A secretary for the office told them King was not available. Rawson said the office would respond to every letter with a return mailing address.
“What we’re asking is that our insurance companies, our insurance commissioner, and everybody who had an obligation in (the 2022 law) just obey the law,” Jones said. “Just do it.”