As Mary Jo Fennell collapsed in the passenger seat from heart failure, her daughter, Conni Burley, checked their location. Eight miles from the local hospital in Sandersville. She turned her car around and drove; emergency room staff stabilized Fennell’s heart with an external pacemaker before putting her on a helicopter to Macon. They saved her life.
“She would not have made it for me to make it to Macon,” Burley said.
Burley and her mom believe the rural Georgia hospital, Washington County Regional Medical Center, mustn’t shut down.
But that’s not out of the question.
Credit: PHOTO by Ariel Hart
Credit: PHOTO by Ariel Hart
Seven rural Georgia hospitals have closed since 2010. Washington County’s is one of 26 others that are at “high financial risk,” according to a new report by the consulting group Navigant. As in many rural hospitals, a significant number of people who walk through the doors have no insurance or low-paying government insurance. People with time to choose and better private insurance drive to bigger cities.
The brutal economics of rural hospitals have come up again and again in the Georgia Legislature over the years. This year, lawmakers are debating a number of bills that have the potential to change the picture.
One measure, Senate Bill 106, with serious momentum and the potential to drive billions of dollars into the state, could give Gov. Brian Kemp the power to help insure hundreds of thousands of Georgians through Medicaid and private insurance. Others would encourage competition in the health care sector, supporters say. Kemp is pushing both approaches.
Groups fighting on both sides of these battles have cited the plight of rural hospitals to make their case.
It’s not just a matter of lives and health of people such as Fennell. If those hospitals fail, already struggling communities lose more jobs and become even less attractive to employers and people. If the state’s rural areas fail, even metro Atlanta may struggle to attract major employers, experts have said. And left to worsen, fixes later will only cost more, an expense that is likely to be borne by taxpayers in metro Atlanta as well. Metro taxpayers already help pay for services in rural areas.
With less than two weeks to go and so much in health care depending on this legislative session, Burley hopes legislators can make the right choices.
Vulnerable
If SB 106 passes, it will give the governor the authority to request “waivers” from the federal government to shape two of Georgia’s health insurance programs. One is Medicaid, the other private insurance under the Affordable Care Act.
Antoine Poythress is watching.
He runs the Sandersville hospital that treated Fennell, 56-bed Washington County Regional Medical Center.
Like Fennell, the majority of the patients who use the hospital are on Medicare or Medicaid, programs health care experts say Congress and the state Legislature have not funded enough to pay the full cost of providing care. Worse still, more than 1 in 10 patients who walk in the door have no health insurance at all.
Those are some reasons why Washington County Regional lost $1.1 million last year.
That’s the good news. The year before that, it lost $4.4 million. And all that after the county voted for a temporary tax increase to save the hospital.
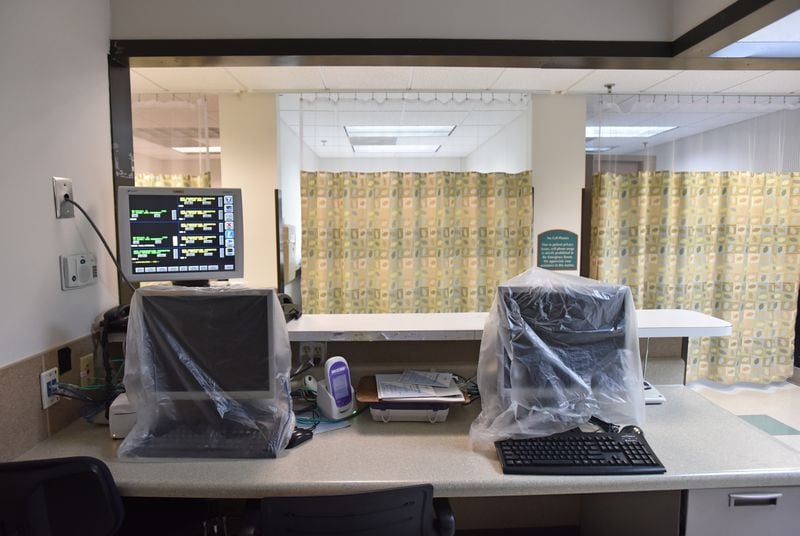
Credit: PHOTO by Ariel Hart
Credit: PHOTO by Ariel Hart
Poythress hopes the Legislature and Kemp will use SB 106 to expand Medicaid to all poor Georgians who are eligible, those up to 138 percent of the poverty level. Kemp has said he will not do that.
"The solution is not more government," Kemp said during his campaign for governor.
But the way Kemp’s office shaped the proposal, it still gives him the authority to expand Medicaid to many thousands of Georgians, those who make up to 100 percent of the poverty level. If Kemp decides to go that far — there’s no indication exactly what he’d do with the waiver — Poythress said he’ll take it.
“Something is better than nothing,” he said.
Some House Democrats don't agree and have opposed the bill because of that.
On the Republican side, the prospect of any expansion has troubled some lawmakers. The powerful president pro tem of the House, state Rep. Jan Jones, told her colleagues to "look very carefully until we add an entirely new entitlement program that doesn't really look at the long-term financial implications."
Either Medicaid expansion or a waiver program would cost the state money. The federal government would pay the majority, bringing billions of dollars into the state health industry either way. But the state would have to help.
For many hospital advocates, the payoff is worth it. Georgia’s rate of uninsured people, 13 percent, is worse than all other states’ except Alaska, Oklahoma and Texas. Its number of closed rural hospitals also nearly tops the charts, along with Texas and Tennessee. Poythress thinks that’s no coincidence.
The uninsured “just don’t pay,” Poythress said.
“That’s some of the battles small rural hospitals are facing because I cannot turn away that patient,” he said.
Neither can big urban hospitals, under federal law. But the difference between him and them, Poythress says, is they can cover the losses with other, better-funded services by tapping their big urban markets of well-insured paying patients.
In Washington County, the patients who can pay and wait often drive to Macon, Augusta or even Atlanta. Washington County Regional is rehabbing facilities, paying for expensive equipment and trying to persuade those patients to stay in Sandersville instead. And persuade the doctors to work there, too. Nine rural Georgia counties have no doctor.
What hospital backers bank on for continuing support is that community leaders know they can’t lose the hospital or the regional industries, such as trucking companies and kaolin processors, will seriously consider shifting operations elsewhere. You can’t attract jobs without a hospital.
“Without this hospital, this community’s got a real problem,” said Dr. Rob Gatliff, Washington County Regional’s general surgeon.
Investing
A couple of hours south of Sandersville, Chris Dorman is the CEO of the Tift Regional Health System and the prosperous Tifton area’s main hospital, Tift Regional Medical Center. It’s not closing any time soon.
Dorman was at pains recently to explain to a state House committee that although the hospital cleared $40 million in operating income last year, it didn’t mean it was rich and the prosperity wouldn’t last. Tift is on track to clear $14 million this year, and out of that it’s paying for projects such as renovations.
That hearing was about another big health care issue that has roiled the hospital industry this session. It’s called certificate of need, or CON. Currently, a health care business that wants to open or expand must obtain a certificate from the state saying their new service is needed. Easing CON would open hospitals up to more competition from private companies.
To entrepreneurs who oppose CON, lifting it would let them innovate, open new clinics and offer patients options.
To Dorman, lifting CON is a way for private businesses to cherry-pick the few profitable services hospitals have, such as outpatient surgery, and leave them with the money-losers, including ER care for people who can’t pay.
Tift has seen it at work. There is already some flexibility in the CON law. And just before Dorman arrived at Tift, three private outpatient surgery centers opened in the area, one right across the street. Tift’s revenue from those procedures fell, he said.
So far, the CON law has withstood a massive lobbying fight between nonprofit hospitals and private businesses. Lawmakers introduced several bills — House Bill 198, Senate Bill 74 and Senate Bill 114 — which all died. But state Rep. Matt Hatchett, the House bill's sponsor, vowed to get the issue moving again before the end of the session, and House Speaker David Ralston told The Atlanta Journal-Constitution he supports that. Kemp this week came out with a forceful statement agreeing. Separately, a more modest CON bill, House Bill 186, passed the Senate Finance Committee on Wednesday.
Some of the biggest supporters for changing or even eliminating CON are rural legislators. They point out the long-standing law has not stopped hospitals in their communities from closing. Those supporters say changes may bring more choices to their areas. Hatchett, for example, sponsored the most sweeping CON bill yet and represents a part of the region served by Washington County Regional. He said that bill would have driven health care prices down for everyone "while protecting our rural service providers."
Credit: HYOSUB SHIN / AJC
Credit: HYOSUB SHIN / AJC
Making a bet
Twenty-five miles from Tifton, the Tift Regional Health System owns another hospital, Cook County Regional Medical Center in Adel. It’s been through a wringer, and it gave up.
About 19 percent of the people treated there had no insurance, not even Medicaid or Medicare. In 2017 it was losing about $2.6 million annually, most of it through the emergency room. Patients who could pay and wait were going out of town.
From the minute Cook Regional CEO Mike Purvis took the job in 2010, he was having talks with the hospital’s owner, then another company, about how much of the hospital to shut down. Purvis was overjoyed when Tift bought Cook because he thought it would try harder to keep serving the community. But even owned by Tift, they still made hard choices.
They eliminated surgery. They quit delivering babies.
Credit: HYOSUB SHIN / AJC
Credit: HYOSUB SHIN / AJC
Then one night in 2017, Dorman, now overseeing both Tift and Cook, drove out to Adel. He, Purvis and Cook’s staff gathered in the small hospital’s emergency room that had treated patients for decades, including Purvis for high school sports injuries. In a little ceremony, they spoke about things like that. Then at midnight, for the first time, they locked the emergency room door. Purvis went to his office and prayed.
The old Cook building still operates temporarily, with some inpatients and a nursing home wing.
Maybe once a week, an emergency case still shows up at the door. Staffers call 911. Emergency medical technicians are a couple of blocks away, and they drive the patients to Tifton or Valdosta.
But Dorman and Purvis have a plan.
Credit: HYOSUB SHIN / AJC
Credit: HYOSUB SHIN / AJC
Cook will be reborn, at a cost of about $50 million. Dorman specializes in health care metrics, and he has convinced his board that there is a way to attract well-insured paying patients: as a brand-new, eye-catching, smartly designed acute care hospital with special geriatric psychiatric services and an emphasis on outpatient surgery, a profitable service. If successful, it will also attract doctors, transforming Cook County into a minor medical employment center.
They’ve also built an urgent care clinic near the old hospital, where 90 percent of the old ER’s patients should have been seen anyway, Purvis said. And the Tift system has left open the option of funding a regular ER in the new Cook hospital.
Dorman presents wholesale CON changes as the one thing that could upend his strategy to bring patients back to Cook.
“It was and still is a scary bet,” Dorman said.
“I’ve always been able to go into an area and grow it,” he said. “What does concern me is, what if everything changes? What if CON goes away?”
Hatchett concedes that CON may have occasionally protected a rural hospital. But he points at hospitals such as Cook to show that CON is not a savior.
“We’ve lost rural hospitals, and it hasn’t done anything to help what we’ve lost,” Hatchett said. “Opening CON allows for more innovation and more competition, and sometimes entities that have existed for years need more competition to improve their existing facilities.”
Why it matters to metro Atlanta
If rural hospitals fail, already struggling communities lose more jobs and become even less attractive to employers and people. Their closures can even cause metro Atlanta to struggle in attracting major employers, experts have said. If the problem is allowed to worsen, fixes later only cost more, with the expense likely borne in part by taxpayers in metro Atlanta who already help pay for services in rural areas.
About the Author









/cloudfront-us-east-1.images.arcpublishing.com/ajc/P7DYBH6TO7FEKG4SUXQQKADRXE.jpg)


