With COVID-19 claiming hundreds of lives across the globe daily, President Trump and a growing number of medical professionals are praising emerging evidence of a potential treatment that uses a well-known malaria medication to stop this virus in its tracks.
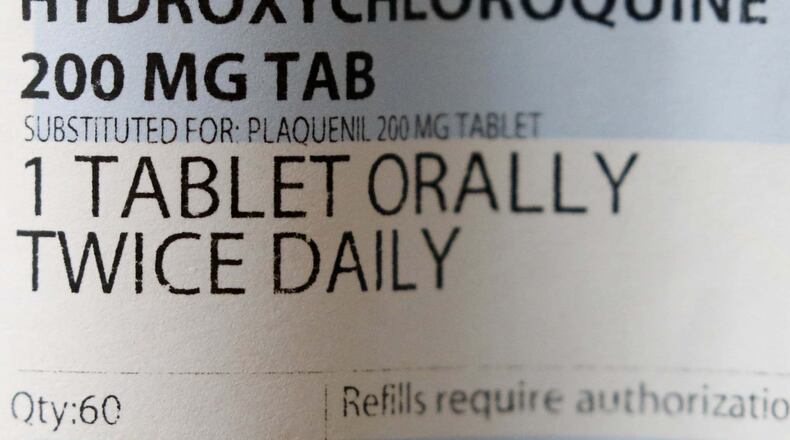
On March 29, the Food and Drug Administration granted emergency approval for the off-label use of hydroxychloroquine after new evidence showed good results for defeating coronavirus in a range of COVID-19 patients.
Meanwhile, pharmaceutical manufacturers are ramping up production of 250 million doses of hydroxychloroquine to be used in the attack against COVID-19.
To be expected, professional regulators and several governors have been skeptical – even putting up roadblocks to compassionate usage for this promising therapy. But in a crisis, it is time to draw on every weapon we have when a patient qualifies and consents to treatment.
Governors in Nevada and Michigan issued orders prohibiting use of the medication. But then Michigan’s governor – who had threatened physicians who prescribed the medication – reversed course and asked for a supply of the medication from the federal government.
The medical community appears to embrace the hope of this drug as well. A survey of more than 1,200 physicians across 50 states by Alpharetta-based Jackson & Coker this week found that 65 percent of the surveyed physicians said they would prescribe the anti-malaria drugs to a family member if they had COVID-19.
Those of us working in healthcare know a great way to get a candid perspective on treatment options is to ask a physician: “Would you give this to your family?”
With the emerging hope from this malaria cocktail, it’s time to put our differences aside and launch the world’s largest, real-time drug trial and save lives at the same time.
The evolution of hydroxychloroquine as a weapon against the coronavirus is one few understand outside the medical profession.
For decades, public health officials distributed a medication named chloroquine to prevent and treat malaria. A close cousin to chloroquine – hydroxychloroquine — is used today to treat conditions such as lupus and rheumatoid arthritis. Some astute scientist observed that lupus patients being treated for malaria received benefit against both.
Over the past few weeks, several randomized controlled trials were conducted to test the effect of chloroquine in treating COVID-19. Therapeutic effects were observed in fever reduction, improvements on chest imaging studies and impeding disease progression.
On March 17, the AIFA Scientific Technical Commission of the Italian Medicines Agency expressed a favorable opinion to include the off-label use of chloroquine and hydroxychloroquine for treating COVID-19.
South Korean health authorities recommended hydroxychloroquine and chloroquine for the experimental treatment of COVID-19.
When options are few, life-and-death decisions must be made with the evidence at hand. That’s how it always works in the emergency department, the surgical suite and the battlefield. Use an off-label weapon such as these medications or go into battle helpless.
Many ER physicians, intensive care doctors, and pulmonologists have already stocked reasonable amounts of hydroxychloroquine for themselves to stay healthy while caring for COVID-19 patients. The existing data are enough for them — even if the FDA wouldn’t have agreed in more normal times.
Dr. Vladimir Zelenko is a board-certified family practice physician who serves the Hasidic Jewish community in Orange County, New York. He has treated more than 700 patients with coronavirus with hydroxychloroquine, azithromycin, and over-the-counter zinc supplements. Not one of his patients has needed ventilation. His recommendation is to prescribe hydroxychloroquine to medium- and high-risk patients in the earliest phase of COVID-19 infection.
We could go a step further with this worldwide, real-time drug trial.
Instead of just treating the sickest patients with chloroquine or hydroxychloroquine, let’s also use these medications to prevent its spread and mitigate illness for those who are exposed. We used them to prevent and treat malaria. Let’s do the same for COVID-19. And then let’s study the results.
Doctors are in the front line treating patients with suspected coronavirus. If doctors believe such medications will protect them or their family members, let’s not wait.
It doesn’t feel right limiting ourselves to handwashing and isolation. All of us want to do more. Let’s embark on the largest clinical trial ever. As Todd Beamer reportedly commanded on United Flight 93, “Let’s roll.”
Jeff Segal, M.D., a neurosurgeon and attorney, is founder and CEO of Medical Justice Services, which works with physicians to protect against professional liability.
About the Author